Content table
There’s a mistaken belief that regular periods equal good fertility health. But that’s not always the case. It’s possible to have regular periods and still have fertility issues.
That’s because periods are only one part of the fertility puzzle. And regular periods are not proof of ovulation.
Many other factors can influence your pregnancy odds. Your reproductive health is affected by your age, lifestyle, underlying health conditions, infections, and much more.
So If you have regular periods but are struggling to conceive, read on. We’ll cover 12 things that can affect your pregnancy chances, and what you can do about them.
Key Takeaways
If you’re struggling to get pregnant, despite having regular periods, know there is hope.
Simple things like cleaning up your diet, managing stress, and tracking ovulation can often have a huge impact on conception. Other times, you may need to consult with your doctor to dig deeper.
To quickly recap, here are the culprits to watch out for that can make it harder to get pregnant:
- Age
- Not trying long enough
- Not timing sex right
- Ovulation problems
- PCOS
- Implantation failure
- Blocked fallopian tubes
- Vaginal infections and STIs
- Male infertility
- Lifestyle factors
- Autoimmune conditions
- Unexplained fertility
If you suspect any of these could be interfering with your fertility, talk with your doctor.
How Do Periods Affect Your Chances of Getting Pregnant?
Your periods help calculate your cycle length, and in turn, your fertile window. Your fertile window is the best time to get pregnant. So nailing your fertile window is a must if you’re TTC.
But your periods also offer hints about your fertility. Generally, regular periods indicate that your reproductive hormones are in balance. That said, periods vary widely from person to person.
So how do you know your cycles are “regular”? Here are some clues:
- Any menstrual cycle between 21 to 35 days is considered regular.
- Menstrual cycles usually last between 2 to 8 days.
- On average, women lose about 60 ml of blood during their menstrual cycle (roughly 4 tbsp.) Anything over 80 ml is considered heavy bleeding.
Irregular cycles and abnormally heavy periods may indicate erratic ovulation. This can both make it harder to get pregnant. So if you’re trying to get pregnant and your periods are outside the norm, it’s essential to talk with your doctor.
Keep in mind, some women have trouble getting pregnant, even if their periods seem A-okay. Which brings up the next question…
Why Am I Not Getting Pregnant When I Have Regular Periods?
If your period arrives like clockwork, but you’re struggling to conceive, there could be several culprits.
Here are 12 reasons you may have trouble conceiving, even if your periods are normal:
Reason #1 – Age
With age, the quantity and quality of a woman’s eggs decline. That’s why it can take longer to get pregnant as you age.
To paint a picture, a woman under 30 has an 85% chance of pregnancy within a year. But once you hit 35, your pregnancy chances drop to 66%. And by 40, those chances sink to 44%.
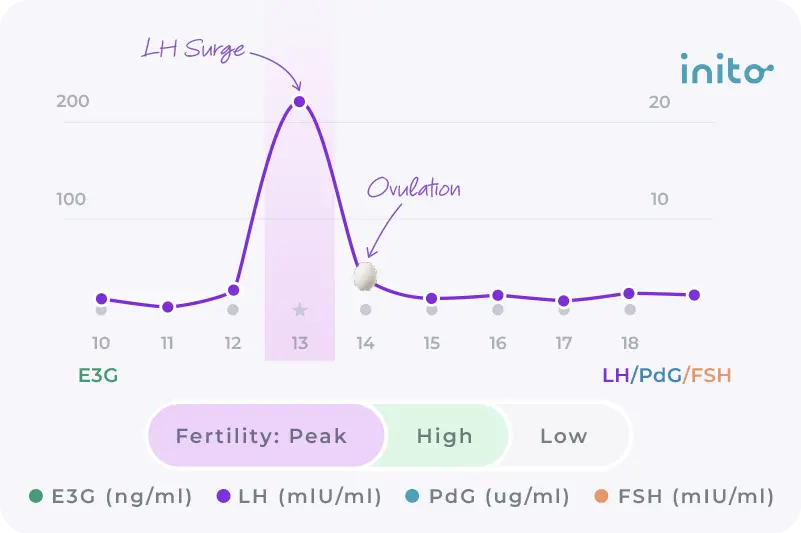
Reproductive hormones also shift with age. FSH (Follicle-Stimulating Hormone) and LH (Luteinizing Hormone) increase, while estrogen and progesterone dip. And this hormonal mix doesn’t provide the ideal setup if you’re trying to get pregnant.
To learn more about how age affects pregnancy, check out: What Are My Chances of Getting Pregnant By Age?
What you can do: While you can’t control your age, you can control your lifestyle. So focus on that. Consume a diet rich in vegetables, fruits, whole grains, legumes, and healthy fats. Regular exercise, stress management, and getting quality sleep can also help maintain hormonal balance.
If you’re over 35 and haven’t gotten pregnant after having unprotected sex for 6 months, consult a doctor. Check your ovarian reserve to plan the next steps.
Reason #2 – Not trying long enough
% of couples | Time taken to get pregnant |
30 | 1 month |
75 | 6 months |
90 | 1 year |
95 | 2 years |
Only 30% of couples get pregnant within the first month of trying. This means expecting those two pink lines right away can be a recipe for disappointment.
The good news? Most couples conceive within one year of trying to get pregnant. Breaking it down further, 75% of couples conceive within 6 months, 90% after one year, and 95% after two years.
While it’s challenging, try your best to remain patient.
What you can do: Keep having unprotected sex for one year, or 6 months if you’re over 35. And be sure to time your babymaking right. [More on this below]
Read More: Getting Pregnant: How Long Does It Take?
Reason #3 – Not timing sex right
Sperm can live inside a woman’s body for up to 5 days. However, an egg only survives 12-24 hours after it is released. So to get pregnant, you’ve got to have sex at the right time.
Having intercourse during the fertile window gives you the best chance of pregnancy. Your fertile window is 6 days long. It consists of the 4 days leading up to ovulation, ovulation day, and the day after ovulation.
As you can see from the chart below, the day before ovulation offers the best chances of pregnancy:
Cycle Day | Chances of pregnancy |
4 days before ovulation | 18% |
3 days before ovulation | 27% |
2 days before ovulation | 33% |
1 day before ovulation | 42% |
Ovulation day | 20% |
1 day after ovulation | 8% |
Read More: When to Have Sex When You’re Trying to Get Pregnant?
What you can do: Pinpoint your fertile window with Inito. The Inito fertility monitor measures LH, FSH, and estrogen to give you a complete picture of your fertility window and PdG (urine metabolite of progesterone) to confirm if you’ve ovulated or not, all on a single test strip. Have unprotected sex every day, or every other day, during your fertile window.
Reason #4 – Not ovulating
As mentioned, regular periods do not confirm ovulation. It’s estimated that for a third of all menstrual cycles, an egg isn’t released. This is known as anovulation – and it’s the #1 cause of infertility.
It’s common to have an anovulatory cycle or two each year. But chronic anovulation can interfere with conception.
Common causes of anovulation include:
- Chronic stress
- Being overweight or underweight
- Excessive exercise
- Polycystic ovary syndrome (PCOS)
- Stopping birth control recently
- Certain medications (including steroid medications and some antidepressants)
What you can do: If you suspect you’re not ovulating, check your progesterone or PdG levels. Progesterone rises after an egg is released. Progesterone’s rise in the luteal phase confirms ovulation. Inito measures your PdG (a urine metabolite of progesterone) to confirm you’re ovulating.
Read More: Anovulation: Everything you need to know about the #1 cause of infertility
Reason #5 – PCOS
Polycystic ovary syndrome (PCOS) is a hormonal imbalance that can cause ovulation problems. Women with PCOS often have excessive levels of androgens (male hormones). This can disrupt menstrual cycles and interfere with the ovulation process. Instead of being released, follicles remain in the ovaries and form cysts.
One of the hallmarks of PCOS is irregular cycles. Yet some women with PCOS still get regular periods. However, that doesn’t mean they’re ovulating.
Regular periods may be accompanied by other symptoms of hyperandrogenism. This includes acne, weight gain, and hirsutism, which is excessive hair growth on the face or body.
That said, not all women have obvious signs of PCOS like weight gain, acne, or facial hair. If your PCOS symptoms are mild, this can lead to a missed diagnosis.
Learn More: PCOS and Pregnancy: All You Need to Know
What you can do: If you have PCOS symptoms like facial hair, acne, or weight gain, visit your healthcare provider. They can do blood work to determine if you have PCOS. And consider using Inito to confirm you’re ovulating.
Reason #6 – Implantation failure
Sometimes the egg gets fertilized but doesn’t implant properly into the endometrium. This is known as implantation failure.
- Implantation failure may be due to:
- Chromosomal abnormalities
- Endometrial receptivity
- Uterine infections
- Hormonal or metabolic disorders
- Thrombophilia
What you can do: Check your progesterone levels. Your body needs adequate progesterone for successful implantation. Visit your doctor to be tested for any underlying medical conditions that can hinder implantation.
Read More: How to Make Implantation Successful: What You Need to Know
Reason #7 – Blocked fallopian tubes
Your fallopian tubes are the pathway connecting your ovaries and uterus. They’re also the meeting point for an egg and a sperm. If this pathway is blocked, so is fertilization.
Blocked fallopian tubes may be due to:
- Endometriosis
- Pelvic inflammatory disease (PID)
- Damage or scarring from previous surgeries
- Sexually transmitted infections (STIs)
Some women with a blocked fallopian tube may feel pelvic pain. Others may experience no symptoms other than infertility.
What you can do: If you’re TTC and all your blood work seems okay, your doctor may suspect blocked fallopian tubes. In this case, they will recommend a hysterosalpingogram (HSP). This is a type of X-ray that can determine whether your fallopian tubes are open or not.
Reason #8 – Vaginal infections & STIs
Untreated vaginal infections can cause inflammation in the genital tract. This may lead to infertility. Inflammation may be caused by endometriosis, bacterial vaginosis, or pelvic inflammatory disease.
STIs like chlamydia or gonorrhea can create scar tissue in the pelvic organs. This can block the fallopian tubes and interfere with fertilization.
Yeast infections can thicken your cervical mucus, making it harder for sperm to swim. They can also alter your vaginal pH and hinder sperm viability.
What you can do: If you suspect you have an STI, see your doctor. They can test and give you the appropriate medication. Consider taking probiotics if you have bacterial vaginosis or a yeast infection.
Reason #9 – Male infertility
It takes two to conceive. And between 40-50% of infertility stems from the male partner.
This could be due to low sperm count or poor sperm motility, meaning sperm have trouble swimming properly. Some sperm may also have head or tail defects that affect their ability to reach and penetrate an egg.
What you can do: Get infertility testing to assess your partner’s sperm.
Reason #10 – Lifestyle factors
Your lifestyle can also throw off your pregnancy odds. If you’re chronically stressed or have insomnia, you’re more likely to face infertility issues.
Stress increases cortisol levels. Cortisol and progesterone are derived from the same precursor, pregnenolone. This means that the more stressed you are, the more pregnenolone is redirected to produce cortisol, rather than progesterone. But it’s not just stress to watch out for.
Smoking cigarettes and drinking alcohol can also reduce fertility. Marijuana affects both male and female fertility. It is linked with a lower sperm count and decreased sperm motility in men. For women, marijuana can lower Luteinizing Hormone (LH), which may affect ovulation.
Your weight also affects fertility. Being overweight or underweight can create hormone imbalances like estrogen dominance, which can lead to ovulatory issues. Generally, BMIs between 18.5 and 24.9 are the sweet spot for conception.
What you can do: Lead a healthy lifestyle. Exercise, eat a nutritious diet, and get 7-8 hours of sleep every night. Keep stress at bay with relaxation techniques like yoga, meditation, or breathwork. Steer clear of alcohol, tobacco, or other drugs.
And if you could use some additional support on your conception journey, consider joining our Facebook community.
Read More: Diet & Fertility: Eat Your Way to Better Baby Odds!
Reason #11 – Autoimmune conditions
Research shows there’s a connection between autoimmunity and infertility. Autoimmune diseases like Hashimoto’s thyroiditis, lupus, and celiac disease make the immune system overactive.
The body produces antibodies that may mistakenly attack the reproductive organs. This can affect your hormones, as well as ovulation and implantation.
What you can do: Talk with your doctor if you suspect you may have an autoimmune condition. And if you do, know that it’s possible to get pregnant with the right diagnosis and treatment.
Reason #12 – Unexplained infertility
Roughly 15 to 30% of couples face unexplained infertility. This is an inability to get pregnant without any clear cause. Meaning, you go through fertility testing, and everyone comes out normal.
Not getting answers can be extremely frustrating. But while you may not pinpoint a cause for unexplained infertility, you can still treat it.
What you can do: Keep trying to conceive for one year if you’re under 35, or 6 months if you’re over 35. After that time, if you still haven’t gotten pregnant, talk to our doctor and consider fertility treatments or artificial reproductive technology (ART).
Summing It Up
Here’s the TL; DR version of what we’ve just covered:
Infertility cause | What can be done? |
Age | Maintain a healthy lifestyle. Keep having unprotected sex for 6 months if you’re over 35. If you’re over 40, consult with a doctor to check your ovarian reserve. |
Not trying long enough | Have unprotected sex for one year, or 6 months if you’re over 35. |
Not timing sex right | Calculate your fertile window with Inito. |
Not ovulating | Check your blood progesterone or PdG (urine metabolite of progesterone) levels if you suspect you’re not ovulating. |
PCOS | If you have acne, weight gain & excessive facial hair, it could be PCOS. Ask your doctor for bloodwork to test for PCOS. |
Implantation failure | Check your progesterone levels. Get testing for thrombophilia, or any uterine infections or abnormalities. |
Blocked fallopian tubes | Get an HSG scan to see if your fallopian tubes are blocked. |
Vaginal infections and STIs | If you have an STI, get the appropriate medications. Take probiotics if you have bacterial vaginosis or a yeast infection. |
Male infertility | Get infertility testing. |
Lifestyle factors | Exercise, eat healthy, get good quality sleep, and manage stress. Avoid smoking and recreational drugs and limit alcohol. |
Autoimmune conditions | Talk with your doctor. |
Unexplained infertility | Keep trying for one year, or six months if you’re over 35. Consider fertility treatments or artificial reproductive techniques (ART). |
When Should I See a Doctor?
As said earlier, if you’re under 35 and have been having difficulty conceiving for a year, visit your OBG-YN. If you’re over 35 and haven’t conceived after six months, see your doctor. And if you’re over the age of 40 and trying to conceive, talk with your doctor right away.
They can help identify any factors that could be interfering with your fertility – or refer you to a fertility specialist if needed.
FAQs
While having a regular period is a good sign, it doesn’t always necessarily mean that you are fertile. Periods are only one factor in your overall fertility. If you want to know if you are fertile, it’s a good idea to confirm whether or not you’re ovulating (the Inito monitor can help with that). You could also consider getting a preconception checkup, which will give you a better idea of how fertile you are.
Here are a few signs that you may have a period that’s irregular:
- Your cycle is less than 21 days or longer than 35 days
- Your menstrual bleeding lasts less than 2 days or longer than 8 days
- Your total volume of blood lost on your menstrual bleed is more than 80 ml (average is closer to 30 ml)
There are quite a few benefits to having a regular period. Firstly, it adds a level of predictability to your month so you can proactively plan things around when you have your period (including when to have sex if you’re TTC). On top of that, a regular period is generally a good sign (though not the only sign) of ovulating and having good hormonal balance.
Signs of an unhealthy period can include:
Heavy bleeding that exceeds more than 80ml over the course of menstruation or passing clots
A period that’s too long or too short (longer than 8 days or less than 2 days)
Too many or two few days between one period and the next (longer than 35 days or less than 21 days)
Very painful cramping or severe mood swings
Bleeding between periods or missed periods
Know more: The 8 Types of Abnormal Menstruation You Should Know About
Here’s a glimpse at what healthy periods look like:
- A normal amount of blood lost (around 30 – 60ml, more than 80ml is considered abnormal)
- Accompanying symptoms that are only mild (like cramping, bloating, etc.)
- Having between 21 – 35 days between periods
- Menstrual bleeding that lasts between 2 – 8 days
There are a few period symptoms that aren’t normal. The first is having extremely heavy bleeding. From day 1 of your bleed to the last day of your bleed, it’s normal to lose around 30 ml of blood; any amount over 80 ml is considered abnormal. Other abnormal symptoms include extreme mood swings that impact daily life, extremely painful cramping, too many or too few days between periods, and a period that’s too short or long (less than 2 days or more than 8).
There are a handful of ways you can tell if your period blood is healthy. First, the color will be bright red for most of your bleed. At times, it may taper off to a pinkish or brownish color. It will not contain large clots (anything larger than a pea). Healthy periods also last between 2-8 days, and the total amount of blood passed should not exceed 80ml. Period blood should also not have any sort of accompanying foul odor (minus the natural scent of blood, of course).
If you have low iron during your period, you’re likely to experience:
- Feeling weak or more tired than usual
- Headaches or dizziness from the loss of blood
- Shortness of breath
- Hands or feet that feel colder than usual
- Pale skin or blood that appears lighter in color than normal
If you think you’re experiencing any of these symptoms, be sure to talk to your doctor.
Was this article helpful?
- The Normal Menstrual Cycle and the Control of Ovulation – Endotext – NCBI Bookshelf
- Heavy periods: Overview – InformedHealth.org – NCBI Bookshelf
- Knowledge about the impact of age on fertility: a brief review – PMC
- ABC of subfertility: Extent of the problem – PMC
- Findings from a mobile application–based cohort are consistent with established knowledge of the menstrual cycle, fertile window, and conception
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4546331/
- Do hyperandrogenic women with normal menses have polycystic ovary syndrome? – Fertility and Sterility
- Bacterial vaginosis and its association with infertility, endometritis, and pelvic inflammatory disease
- Trends of male factor infertility, an important cause of infertility: A review of literature – PMC
- Full article: The relationship between stress and infertility
- Infertility in women and moderate alcohol use. – PMC
- Associations between smoking status and infertility: a cross-sectional analysis among USA women aged 18-45 years – PMC
- Effects of marijuana on reproductive health: preconception and gestational effects – PMC
- Diagnosis and Treatment of Unexplained Infertility – PMC