Content table
Most people enter TTC feeling unprepared. But there’s another side to TTC stories: the doctors.
The doctors, specialists, and embryologists who guide others through the process while quietly navigating their own. They read the labs, interpret the hormones, and explain the cycles. And then they go home and face the same fertility driven uncertainty their patients do.
Training gives them clinical language. Lived experience fills in what textbooks miss. That dual lens reveals the gaps, where support falls short and patients need more than reassurance. They need insight.
Three experts. Three lived experiences. One shared truth: seeing both sides of the exam table rewires how you think about care.
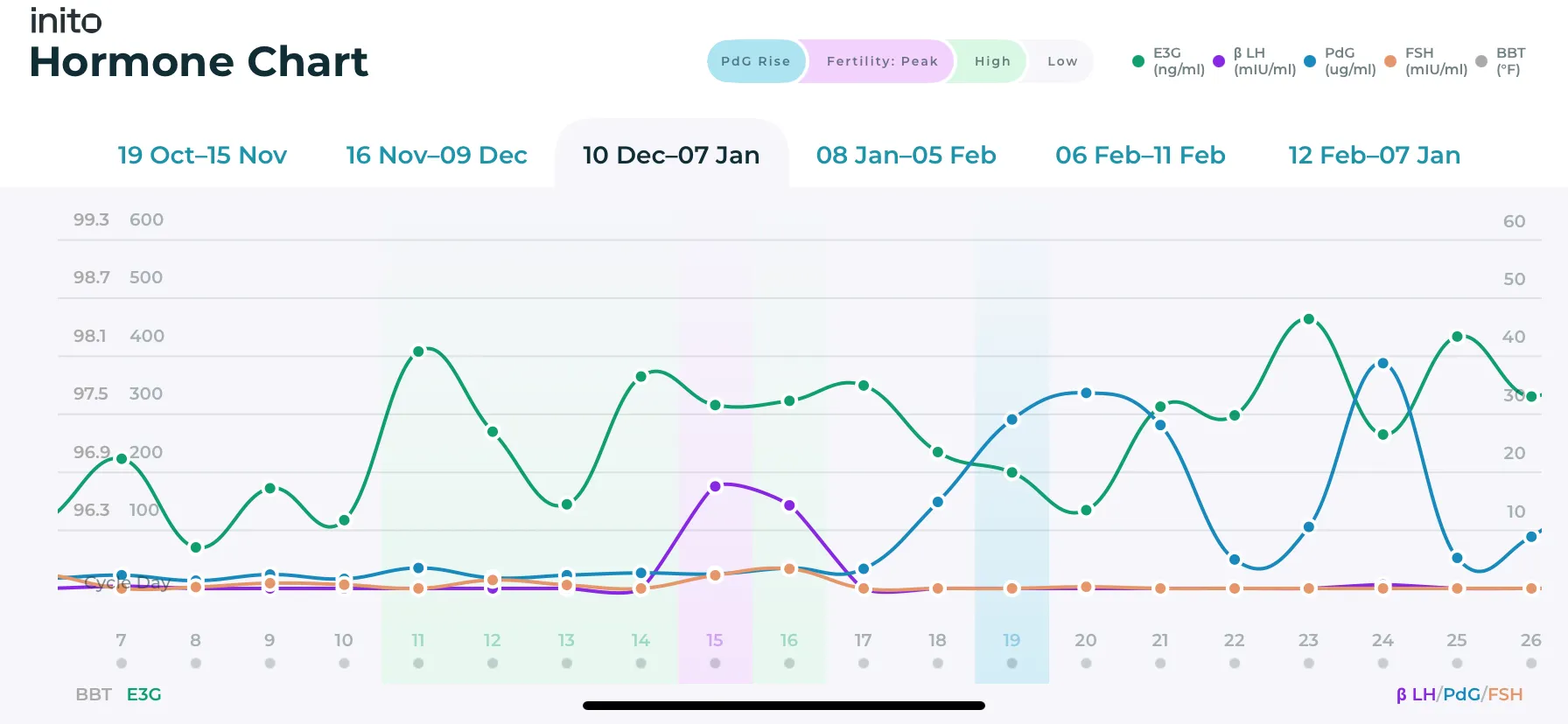
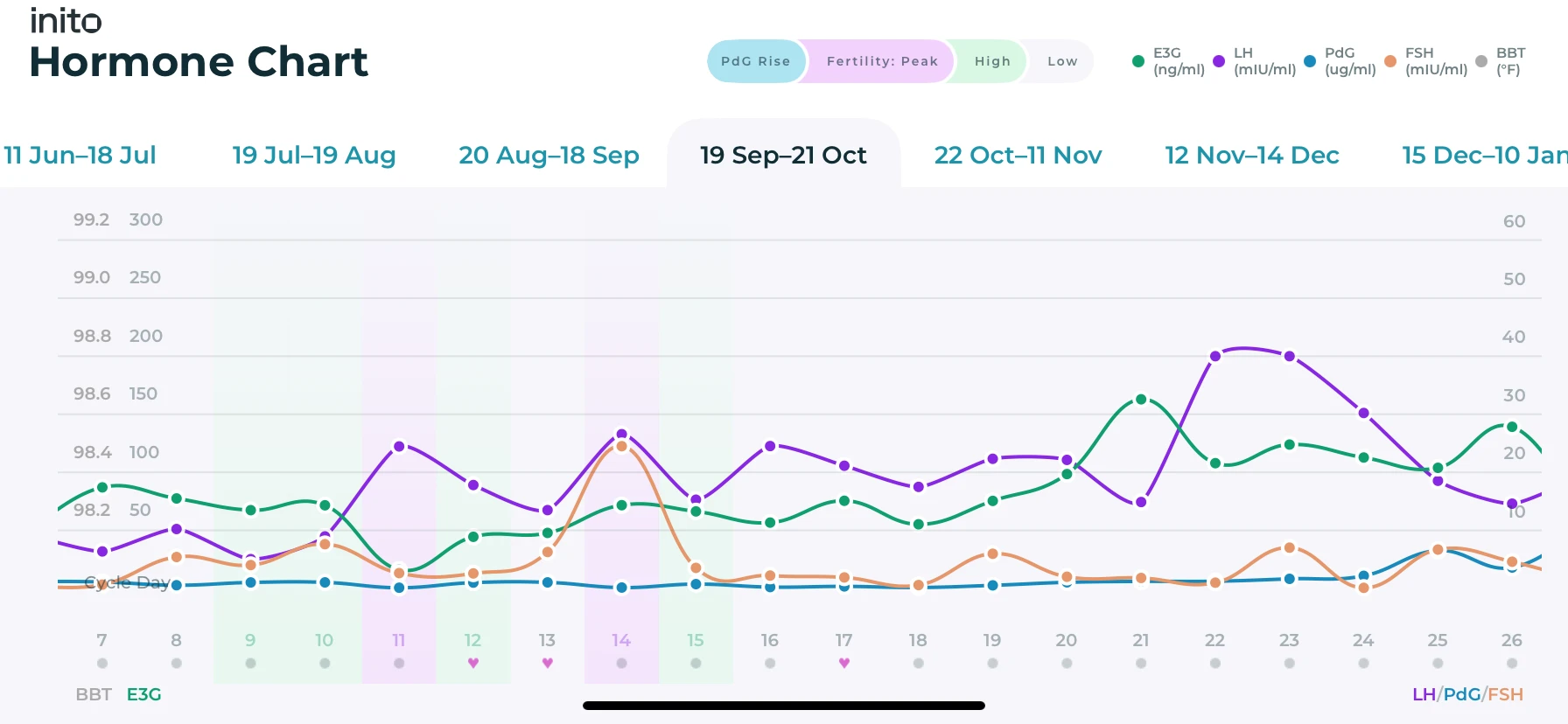
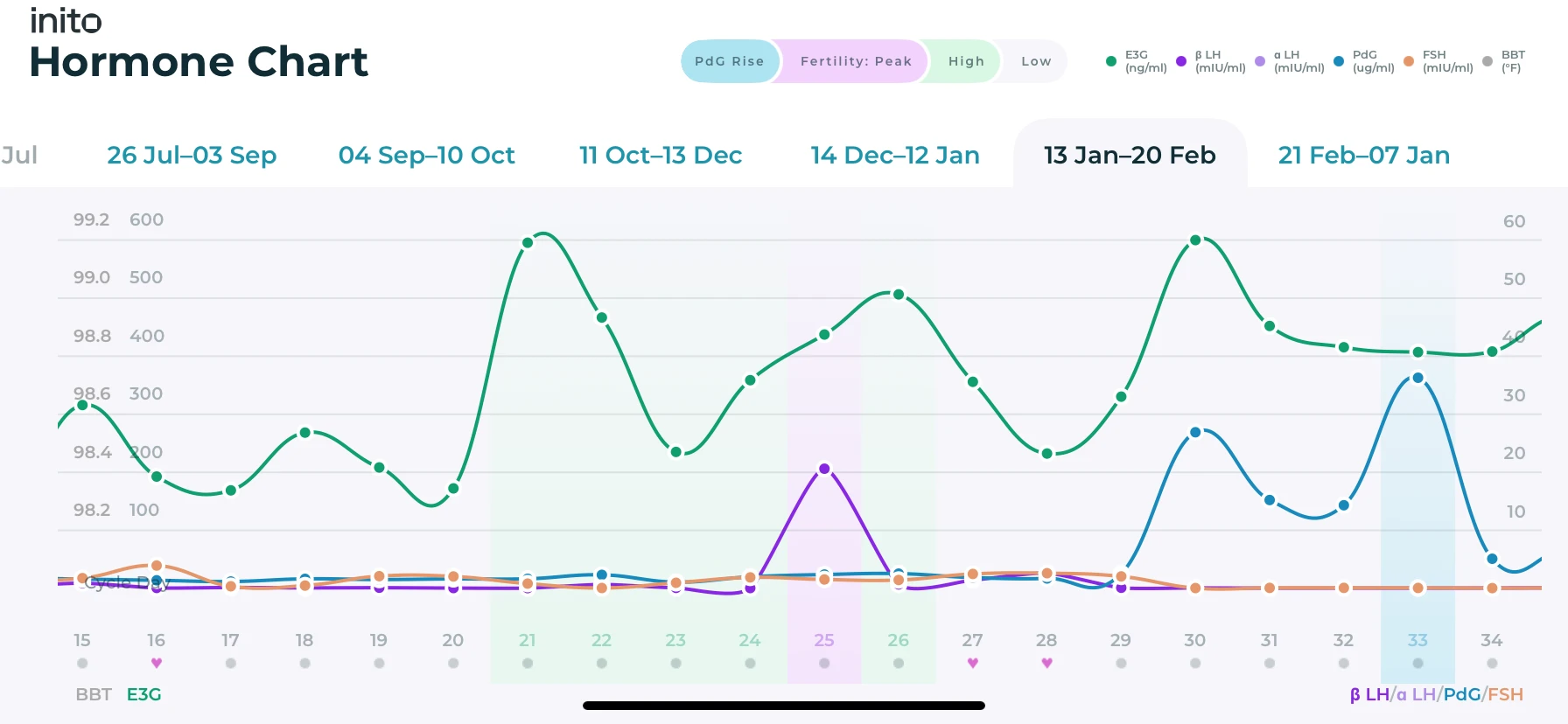
Disclaimer: Charts shown are illustrative and do not represent the actual data of individuals featured.
When the Doctor Lives the Diagnosis: Dr. Roxanne Pero
After more than 14 years as a board-certified Ob-Gyn, Dr. Roxanne Pero spent her days delivering babies while privately navigating her own long road to pregnancy. She still remembers the moment her intuition cut through the noise: “Even though I was having regular periods, something just felt off.” Her experience would later become one of the many TTC stories patients quietly look for when they enter her office hoping someone might finally understand.

Her journey stretched across four years of treatments, setbacks, and loss. “We went through a very long fertility journey,” she says. Four years of trying, grieving, and starting again. It wasn’t just medical. It was the quiet weight between cycles. Trying to conceive after miscarriage. After failed attempts. After hope kept rebuilding and breaking. “You feel like everyone around you is getting pregnant,” she says. “Everyone but you.”
Living through that changed how she practiced medicine. As both doctor and patient, she became deeply attuned to the questions women carry quietly. “I have so many questions about what’s going on inside my body,” they tell her. Words she once said herself. She also understood why standard tools often fall short. “Most women don’t fit the statistical average.”
Everything shifted when she could finally see her hormone patterns clearly. Not symbols. Not guesses. “With Inito, you can see your actual hormone values,” she says. That clarity, especially around confirming ovulation through tracking PdG (the urine metabolite of progesterone), changed everything. Today, she uses that insight to adjust timing, spot anovulation early, and move forward with confidence. “It’s incredibly empowering,” she says. “Once you have the information, you can do something about it.”
Now, her medicine is shaped by lived experience as much as training. She walks beside women with their own numbers, their own patterns, their own story.
Because hope isn’t one size fits all.
When the Gaps Become Visible: Dr. Franziska Haydanek
As an OB-GYN living with PCOS, Dr. Franziska Haydanek has stood on both sides of the exam table. When she was diagnosed with PCOS she remembers thinking, “I didn’t know what that meant for me… I was fearful that it meant I may never be able to have [children].” That fear shaped how she listens to patients whose TTC stories often begin long before they enter her office. Many arrive carrying notebooks full of ovulation strips, confusion, and weeks of guesswork.
Day-to-day practice exposed the problem: traditional tests can hint at a hormone surge but cannot confirm ovulation. “My patients get incredibly frustrated… they’re doing everything that I’ve asked them to do and we’re still not getting any answers,” she says. Those notebooks became a record of hope and uncertainty, taped strips that rarely answered the core question: did ovulation actually happen? It’s a familiar pattern across ttc after miscarriage, ttc with pcos stories, and anyone navigating early infertility.
The turning point came when a patient opened an app instead of a binder. Seeing hormone graphs, cycle by cycle, gave Dr. Fran a living timeline she could actually work with. For the first time, hormone tracking offered clarity without guesswork. Where lab visits and single-day bloodwork left gaps, continuous tracking filled them. Patterns emerged. Decisions became grounded. Care shifted from reactive to iterative.
One patient made it real. After diagnosis, targeted changes, and month-by-month tracking, she conceived. Pregnancy confirmed.
That moment reshaped Dr. Fran’s practice. Data became a companion to care, not a replacement for it. Hormone tracking turned waiting into measurable progress. When the invisible becomes visible, agency replaces uncertainty, and hope becomes empathy in practice.

Insights Shape Journeys: Alease
Inside the lab, embryologists see names before they see faces. Alease meets women when something hasn’t worked yet. And every time, she hopes she won’t see that name again.
“We’re behind the scenes, but we ride the highs and lows with them,” she says. “There’s nothing like seeing someone bring in the little one you helped make.” Her days are filled with quiet, unseen TTC stories, each one waiting for a shift.

She sees the gap long before treatment begins: no real reproductive education, no clear sense of what a healthy cycle looks like, and no clarity in the moments that matter most. Her turning point wasn’t in the lab. It was a friend texting faint test strips, asking if they meant anything. “We’re told our whole lives how not to get pregnant,” she explains, “but no one teaches us what a normal cycle even looks like.”
When she found Inito she sent it immediately. Her friend finally felt like she was tracking something real. No more guessing, no more holding test strips up to the light. With real hormone tracking along with tracking PdG (the urine metabolite of progesterone), the noise fell away. “Women are doing everything right,” Alease says, “they just haven’t been given the information they deserve.”
For Alease, knowledge isn’t abstract. It’s agency. It changes conversations in the clinic, reshapes decisions, and shortens the path to the right care. It turns confusion into something usable. “For women that have gone through lots of fertility struggles and all the trauma that comes with that. It’s really such a miracle that we have this information that they can feel like they’re in control of their cycle, of their journey, because that control is everything. For someone who didn’t feel like they had it before.” These are the moments that eventually become ttc success stories, even if they start in uncertainty.
And in all of it, she returns to the same truth: hope is resilient.
Hope is radical when it’s informed
The shift didn’t come from a grand revelation. It came from the smallest moments. Ones that stayed.
A patient showing Dr. Fran a full hormone chart instead of a notebook of strips. She’s now 33 weeks pregnant.
A friend texting Alease the same faint lines over and over, until she handed her a tool that finally broke the pattern.
Dr. Pero realizing that clarity doesn’t require invasive procedures. It requires visibility — especially for women who fall outside the “average.”
Together, their experiences point to the same outcome: real hormone insight isn’t a luxury. It’s a catalyst. It gives clinicians better judgment. It gives patients control. It replaces the waiting with direction.