Content table
Heard of FSH and LH? If you’re trying to conceive, chances are you have! Follicle-stimulating hormone (FSH) and luteinizing hormone (LH) both play a key role in fertility.
Without normal levels of FSH and LH, you can’t get pregnant. Yet the ratio between these hormones can also affect your chances of pregnancy.
If LH is disproportionately higher than FSH, you could have PCOS. And if it’s the other way around, it could mean you’re short on eggs. Either way, it can make it tough to get pregnant.
But don’t worry! In this article, we’ll cover everything you need to know about the FSH and LH ratios – including how they are measured and what you can do to get them in a normal range.
But first, let’s explore what these hormones do…
Functions of FSH
Follicle-stimulating hormone (FSH) is a reproductive hormone made by your pituitary gland. It helps in keeping your menstrual cycle regular and plays an important role in fertility.
At the start of your cycle (the follicular phase), FSH stimulates the development of your ovarian follicles. Inside each follicle lies an egg, or oocyte.
As the follicles grow, eventually the biggest, healthiest one takes over. This is known as the dominant follicle. This mature follicle then goes on to secrete estrogen.
Once estrogen rises, FSH drops to prevent another follicle from developing. Estrogen’s rise also triggers luteinizing hormone (LH) to increase. More on LH later…
Why should you measure FSH?
|
Female age |
Number of eggs |
|
In-utero |
6-7 million |
|
Birth |
1-2 million |
|
Puberty |
300,000-500,000 |
|
37 years old |
25,000 |
|
51 years old |
1,000 |
Since FSH is in charge of stimulating follicle development, its levels vary depending on how many follicles you have left. If there are plenty of high-quality eggs present, not much FSH is needed to stimulate them.
However, if there are fewer eggs left, or if the quality is poor, more FSH is needed to stimulate the follicles to grow. That’s why high FSH levels are considered a sign of low ovarian reserve.
Learn More: Boost Your Ovarian Reserve: How to Reduce High FSH Levels
Functions of LH
Like FSH, luteinizing hormone (LH) is also secreted by your pituitary gland. LH serves as the spur that sets ovulation in motion.
As mentioned, when estrogen rises, it triggers LH to spike. This surge in LH causes the mature follicle to rupture, releasing the egg. No LH surge = no ovulation.
See how your hormone chart might look like!
Answer some questions to help us provide you a free personalized hormone chart customized to your hormonal health and conditions
Why should you measure LH?
In short? Because it can help you get pregnant! LH begins rising around 24-36 hours before ovulation. The egg is released within 8-20 hours of the LH peak.
Conception is all about timing. Sperm can survive within a female’s reproductive tract for up to 5 days. But an egg only lasts for 12-24 hours once released. If sperm are on hand when the egg is released, you’ll have a better shot at conceiving.
Measuring your LH levels helps you predict when ovulation is coming. That way you know the best time to get busy when you’re trying to conceive.
Learn More: LH Levels & Surges: What’s a ‘Normal’ LH Level Look Like?
So to sum it up…
- FSH helps your follicles develop
- Estrogen signals that the follicle is mature
- LH helps release the egg
FSH and LH both offer important insights about your reproductive health on their own. But their ratio can give valuable clues as well.
How are FSH and LH measured?
FSH blood testing levels
|
Cycle phase |
FSH serum levels |
|
Follicular phase |
1.4-9.9 mIU/mL |
|
Ovulatory peak |
6.2-17.2 mIU/mL |
|
Luteal phase |
1.1-9.2 mIU/mL |
|
Postmenopausal |
19.3-100.6 mIU/mL |
LH blood testing levels
|
Cycle phase |
LH serum levels |
|
Follicular phase |
1.68-15 mIU/mL |
|
Midcycle peak |
21.9-56.6 mIU/mL |
|
Luteal phase |
0.61-16.3 mIU/mL |
|
Postmenopausal |
14.2-52.3 mIU/mL |
FSH urine testing levels
|
Cycle phase |
FSH urine levels |
|
Follicular phase |
0-10 mIU/mL and peaks up to 25 mIU/mL |
|
Luteal phase |
0-10 mIU/mL |
LH urine testing levels
|
Cycle phase |
LH urine levels |
|
Follicular phase |
0-5 mIU/mL and peaks at 10-50 mIU/mL |
|
Luteal phase |
0-5 mIU/mL |
FSH blood testing levels
|
Cycle phase |
FSH serum levels |
|
Follicular phase |
1.4-9.9 mIU/mL |
|
Ovulatory peak |
6.2-17.2 mIU/mL |
|
Luteal phase |
1.1-9.2 mIU/mL |
|
Postmenopausal |
19.3-100.6 mIU/mL |
LH blood testing levels
|
Cycle phase |
LH serum levels |
|
Follicular phase |
1.68-15 mIU/mL |
|
Midcycle peak |
21.9-56.6 mIU/mL |
|
Luteal phase |
0.61-16.3 mIU/mL |
|
Postmenopausal |
14.2-52.3 mIU/mL |
FSH urine testing levels
|
Cycle phase |
FSH urine levels |
|
Follicular phase |
0-10 mIU/mL and peaks up to 25 mIU/mL |
|
Luteal phase |
0-10 mIU/mL |
LH urine testing levels
|
Cycle phase |
LH urine levels |
|
Follicular phase |
0-5 mIU/mL and peaks at 10-50 mIU/mL |
|
Luteal phase |
0-5 mIU/mL |
One easy way to check your FSH and LH levels is to use the Inito Fertility Monitor. Inito tracks your FSH, LH, estrogen, and PdG (a urine metabolite of progesterone) all on a single test strip.
Testing this unique combo helps you pinpoint your fertile window and confirm whether ovulation really happened.
Note: To calculate your FSH: LH ratio, you’ll need your blood values. While urine values are helpful, they can’t be used to calculate the ratio.
What is a normal LH to FSH ratio?
In healthy women, the LH to FSH ratio is usually between 1 to 2. But since your hormones shift with your menstrual cycle, so does your LH: FSH ratio.
At the beginning of your cycle (the follicular phase), the LH to FSH ratio is closer to 1:1, meaning you have roughly the same amount of these hormones.
Then, just before ovulation as LH increases, so does the ratio. As LH falls in the luteal phase, the ratio goes back towards 1 to 1.
See how your hormone chart might look like!
Answer some questions to help us provide you a free personalized hormone chart customized to your hormonal health and conditions
What does an increased LH: FSH ratio mean?
Often, it’s a sign of polycystic ovarian syndrome (PCOS). In fact, about 60% of women with PCOS have an increased LH: FSH ratio.
The LH to FSH ratio in PCOS may be as high as 2:1 or even 3:1, meaning LH is two to three times higher than FSH.
Polycystic ovary syndrome (PCOS) is a condition where there is a hormonal imbalance, and this causes cysts to form in the ovaries of some women. These fluid-filled sacs are actually follicles that are meant to mature and release an egg. But in PCOS, these follicles don’t develop.
Women with PCOS tend to have high levels of male sex hormones (known as androgens). They also often have high levels of estrogen and LH, as well as problems with insulin resistance.
Many women with PCOS have low to normal FSH levels, but higher LH levels. This is known as an elevated LH to FSH ratio.
As mentioned, LH usually surges 12-14 days before your next period to trigger the egg’s release from the follicle. But since LH levels stay high in PCOS, the surge doesn’t necessarily cause ovulation.
Without an adequate LH surge, ovulation can’t occur (known as anovulation). That’s why anovulatory cycles are common in women with PCOS.
So, how can you track and confirm ovulation with PCOS?
Well, since LH levels are always high in PCOS, this can be tricky.
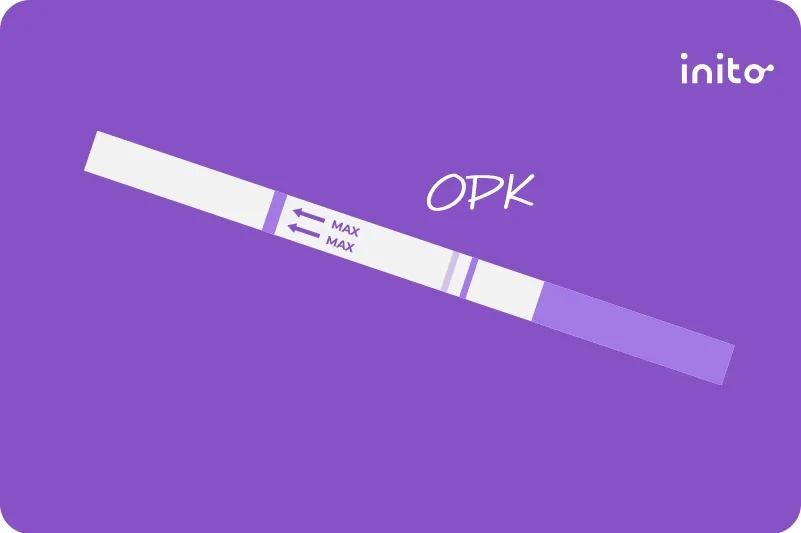
Most ovulation predictor kits (OPKs) base their results on average thresholds (usually 25 mIU/mL). If your LH is over that mark, the OPK will give you a positive result.
But if you have PCOS, your LH could be above 25 mIU/mL your entire cycle! As you can see, this can easily lead to a false positive. That’s why it’s best to use quantitative tests that show your real hormone levels.
Inito measures your actual numerical values of FSH, LH, and estrogen to identify your fertile window. And unlike most OPKs, Inito also measures PdG, a metabolite of progesterone.
Progesterone (and its metabolite PdG) rises after the release of an egg. So it’s the only hormone that can confirm ovulation. Since women with PCOS don’t always ovulate every month, checking progesterone metabolite PdG is key.
What does an increased FSH: LH ratio mean?
If your FSH levels are much higher than LH, it may suggest decreased ovarian reserve.
As mentioned, your ovarian reserve is how many viable eggs are available for fertilization. The fewer eggs you have left, the more FSH is needed to stimulate the remaining follicles.
In the early follicular phase, if your FSH to LH ratio is high, it’s a sign you may respond poorly to ovarian hyperstimulation.
However, your ovarian reserve can’t be assessed by FSH alone. Other markers of ovarian reserve need to be considered too, like anti-Mullerian hormone (AMH) and antral follicle count. You can learn more about AMH here.
How important are the ratios if I’m trying to get pregnant?
It’s not entirely clear. But here’s what some of the data says.
Elevated FSH to LH ratio
One study found women who had an FSH: LH ratio over 2 on day three of their cycle had poorer outcomes from IVF treatment. This included fewer follicles, fewer eggs, and fewer embryos.
Elevated LH to FSH ratio
In the past, doctors used this ratio to help diagnose PCOS. But the research is mixed.
Evidence shows a high LH to FSH ratio is linked with higher androgen levels, a hallmark sign of PCOS. However, other research suggests the LH: FSH ratio isn’t an accurate method for diagnosis. PCOS is usually diagnosed by irregular menstrual cycles, high levels of androgens, and the presence of ovarian cysts on ultrasound.
So while you can’t diagnose PCOS from an abnormal LH to FSH ratio alone, it can offer useful insights.
When should I get my ratio tested?
Your doctor may want to test your LH to FSH ratio if you have signs of PCOS such as:
- Irregular menstrual cycles
- Signs of high androgen levels like acne, facial hair growth, or hair loss that resembles male pattern balding
- Insulin resistance symptoms such as high BMI, skin tags, or patches of dark skin
- Difficulty getting pregnant
You may also want to check your FSH to LH ratio if you’re over the age of 40 and trying to get pregnant. This can offer clues about your ovarian reserve to gauge how much reproductive potential you have left. That way, you can make informed decisions on your conception journey.
But remember, the ratio should never be used in isolation. It should always be used in conjunction with other assessment tools.
How can I get my ratio back to normal?
You can’t always. But it all depends on which hormone is higher – your FSH or LH.
Increased FSH: LH ratio (high FSH levels compared to LH)
Age is the most common culprit of high FSH levels and diminished ovarian reserve. In fact, it’s totally normal! Clearly, this one’s out of your hands.
But age doesn’t always throw off the ratio. In perimenopausal women, FSH rises, but so does LH. This is because estrogen and progesterone drop in perimenopause, causing LH to increase.
For this reason, sometimes the FSH: LH ratio isn’t dramatically different for some women in perimenopause.
It’s also important to note that if you’re undergoing IVF and have a high FSH to LH ratio, lowering it won’t always improve your fertility. You could have an underlying health issue going on that needs treatment. If you suspect something deeper is going on, talk with your doctor.
Increased LH: FSH ratio (high LH levels compared to FSH)
Before we dive into how to improve your LH: FSH ratio, let’s clear one thing up. While doctors use LH to FSH ratios to help diagnose PCOS, the ratio alone is not grounds for diagnosis. It simply gives you a snapshot of your hormones, so you know if further digging is needed.
If you learn that you do have PCOS, take a deep breath and know that it is manageable. Sometimes a few dietary and lifestyle changes are all it takes to restore hormone balance and reduce your PCOS symptoms.
For many women, the first step in treating PCOS is to lose weight. PCOS is linked with insulin resistance, which is when the body doesn’t respond well to insulin. And research shows that as body fat increases, so does your risk of insulin resistance.
This may explain why 40-80% of women with PCOS are overweight or obese. And you don’t need to do any fad diets or go to extremes. Losing even 5-10% of your body weight helps reduce symptoms.
But we know this is easier said than done. So here are a few ways to support weight loss with PCOS:
Exercise
Exercise is proven to reduce insulin resistance and help women with PCOS lose weight. And any exercise helps! The trick is to pick something you enjoy, so you stick with it. Aim for 150 minutes or more of moderate exercise each week.
Reduce refined carbs
To improve insulin sensitivity, try cutting back on sugar and reducing your intake of refined carbs. Refined or simple carbs like white bread, pastries, and white rice have fewer nutrients and fiber. Because of this, they can spike your blood sugar, which can lead to insulin resistance.
Instead, replace them with complex carbs like fruits, vegetables, oatmeal, brown rice, and legumes.
Anti-inflammatory foods
The anti-inflammatory diet is shown to improve hormone balance and restore menstrual regularity in women with PCOS. The anti-inflammatory diet focuses on foods that lower inflammation such as:
- Berries
- Fatty fish like salmon, sardines, & mackerel
- Leafy greens
- Tomatoes
- Nuts
- Extra virgin olive oil
- Herbs and spices, such as turmeric, cinnamon, garlic, ginger, and rosemary
Seed cycling
Many claim this wellness trend can help balance your estrogen and progesterone and lessen PCOS symptoms. Seed cycling involves eating certain seeds during set phases of your menstrual cycle.
While there’s no scientific research to back this method up (at least not yet), many swear by it. And it sure can’t hurt! To learn more about seed cycling, check out this post.
Medications
If you try the lifestyle habits above but still aren’t ovulating, you may want to speak with your doctor. Certain medications can help induce ovulation in women with PCOS. Your doctor may prescribe Clomid, Metformin, Letrozole, or gonadotropins to help you ovulate.
Takeaways
- Follicle-stimulating hormone (FSH) is in charge of helping your ovarian follicles develop.
- Luteinizing hormone (LH) triggers your ovaries to release the egg.
- The relationship between FSH and LH (or the FSH and LH ratios) can help you understand your fertility better.
- A normal LH: FSH ratio is between 1 to 2, depending on the phase of your menstrual cycle.
- An elevated FSH to LH ratio is a sign of diminished ovarian reserve, which means you may not have many eggs left, or their quality may be poor.
- An elevated LH to FSH ratio is common in women with PCOS. But you can’t base diagnosis only on the ratio.
- You can track your FSH and LH levels by blood or urine testing to help calculate your ratio.
- Inito allows you to check both of these hormones from the comfort of your home, along with estrogen and PdG (a metabolite of progesterone). This helps you identify your fertile window and confirm you actually ovulated.
- You can improve your LH to FSH ratio by shifting your lifestyle. Exercising regularly, reducing carbs, and eating more anti-inflammatory foods can help you lose weight and relieve PCOS symptoms.
Was this article helpful?
- Embryology, Ovarian Follicle Development – StatPearls – NCBI Bookshelf
- Female Age-Related Fertility Decline | ACOG
- Follicle-Stimulating Hormone – Health Encyclopedia – University of Rochester Medical Center
- Luteinizing Hormone (Blood) – Health Encyclopedia – University of Rochester Medical Center
- Follicle Stimulating Hormone (LH: FSH) Ratio in Polycystic Ovary Syndrome (PCOS) – Obese vs. Non- Obese Women
- Elevated baseline LH/FSH ratio is associated with poor ovulatory response but better clinical pregnancy and live birth in Chinese women with PCOS after ovulation induction – PMC
- Fertility With Early Reduction of Ovarian Reserve – PMC
- Elevated day 3 follicle-stimulating hormone/luteinizing hormone ratio ≥ 2 is associated with higher rates of cancellation in in vitro fertilization-embryo transfer cycles – Fertility and Sterility
- Luteinizing Hormone to Follicle-Stimulating Hormone Ratio Significantly Correlates With Androgen Level and Manifestations Are More Frequent With Hyperandrogenemia in Women With Polycystic Ovary Syndrome | Morshed | Journal of Endocrinology and Metabolism
- The LH/FSH ratio has little use in diagnosing polycystic ovarian syndrome
- Obesity and insulin resistance – PMC
- Obesity and Polycystic Ovary Syndrome – PMC
- Implementing the international evidence-based guideline of assessment and management of polycystic ovary syndrome (PCOS): how to achieve weight loss in overweight and obese women with PCOS? – ScienceDirect
- Metabolic syndrome, diet and exercise
- Anti-Inflammatory Dietary Combo in Overweight and Obese Women with Polycystic Ovary Syndrome – PMC