Content table
Think you may be experiencing perimenopause symptoms? Or wondering what you can do to actually get some relief? You’re far from alone!
Perimenopause is a period of notorious hormonal changes and uncomfortable symptoms for women. In fact, some studies estimate that 90% of premenopausal women seek medical care for their unwanted symptoms.
So let’s dive into specific perimenopause symptoms to look out for and ways you can loosen their hold on you.
Key Takeaways
- Perimenopause is the transition period when you begin changes that phase you out of being able to reproduce.
- This gradual transition usually starts in a woman’s mid-40s and lasts around 7 years. It brings on lots of hormonal changes and also uncomfortable symptoms for many women.
- The most common pre-menopausal symptoms are irregular periods, hot flashes, night sweats, vaginal changes, and sleep problems. But other menopausal symptoms include nausea, weight gain, tender breasts, and fertility struggles.
- Most of these symptoms are triggered by your natural estrogen levels decreasing. These estrogen changes are triggered by the steady decline in your ovarian reserve (the number of healthy eggs you have left).
- If you struggle with pre-menopause symptoms, there are a variety of ways to find relief. From lifestyle changes, hormone replacement therapy to symptom-specific remedies, there’s hope!
- Talk to your doctor about your specific symptoms for more individualized guidance.
- You can still get pregnant even if you’re already in perimenopause. (This is because you’re still likely ovulating in at least some of your cycles.)
- If you’re trying to conceive and you’re perimenopausal, check in with your doctor to discuss your fertility goals.
What Is Perimenopause? How Is It Different From Menopause?
First, a quick refresher on what exactly perimenopause is.
Peri means “around.” So perimenopause refers to the years when you are around or approaching menopause.
It’s a transitional period where a woman’s body is phasing out of her fertile reproductive years.
For most women, perimenopause lasts around 7 years, but it can go on for up to 14 years. You officially transition from perimenopause to menopause once you’ve gone 12 months without a period.
The exact timing of perimenopause varies from woman to woman. But a telltale sign you’re entering perimenopause is when you have menstrual irregularities. This often starts in a woman’s mid-40s, though it can onset as early as your 30s or as late as your 50s.
Medical professionals and researchers are still learning more about this transitional period. So for the time being, perimenopause isn’t all that well-defined.
But for a better glimpse into exactly what’s going on internally during this transition, keep reading!
What Happens During Perimenopause?
A lot is going on behind the scenes with your hormones and reproductive organs.
First, as you age, the quality and quantity of your ovarian follicles decline. As this happens, your levels of naturally circulating estrogen also go down.
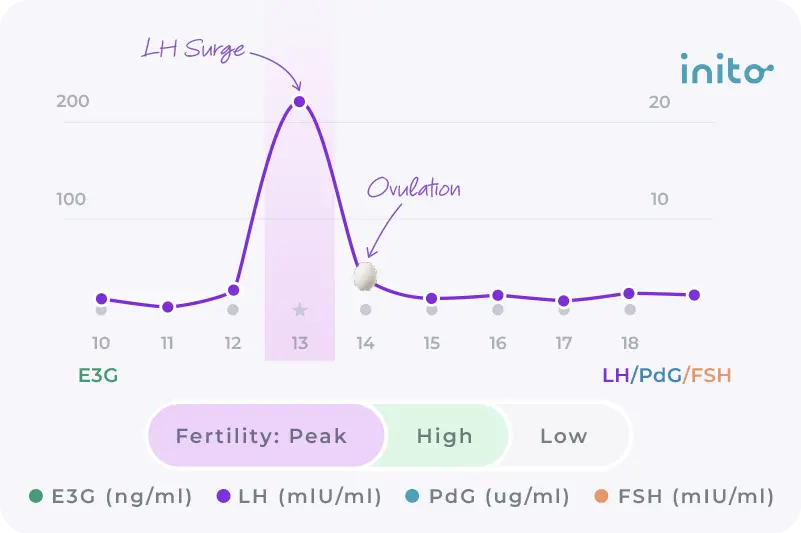
This dip in estrogen levels causes your menstrual cycles to become less regular. This is why you may begin to have cycles where you don’t ovulate at all (aka anovulatory cycles).
When this happens, your FSH (Follicle-Stimulating Hormone) and LH (Luteinizing Hormone) work even harder. They do this in an attempt to trigger the growth and release of ovarian follicles.
And because your egg supply is continually decreasing, your levels of AMH (Anti-Muellerian Hormone) get lower too.
Thanks to all these changes in hormone levels, you begin to experience perimenopausal symptoms.
Of course, these changes don’t happen all at once. They may even be rather subtle at first. But it helps to understand how the gradual stages of perimenopause unfold. (This way you won’t be shocked or surprised when it all goes down.)
What Are the Stages of Perimenopause?
Perimenopause can be separated into two major stages:
1. Early perimenopause
In this stage, you may see your cycle length change by more than 7 days from one cycle to the next.
2. Late perimenopause
In this second stage, your cycles become even stretched out with more than 60 days between cycles.
Whether you’re in early or late perimenopause, you’re likely to experience physical and emotional symptoms. Keep reading to see the most common perimenopausal symptoms to watch out for!
Common Symptoms of Perimenopause
You may not experience these symptoms all at once. But below are the major symptoms that women experience at various points during perimenopause.
1. Irregular periods
The irregularity of your periods is the most definitive sign of perimenopause. It’s why it’s used to mark whether you’re in early or late perimenopause.
The time between one period and the next becomes more unpredictable due to changes in your estrogen levels. This can cause you to experience unexpected bleeding, perimenopause spotting, and even anovulation.
Know more: Perimenopause Spotting When Wiping: Is it Normal?
As far as your menstrual period goes, the heaviness of your flow fluctuates and you may have missed or skipped periods.
2. Hot flashes
Somewhere between 30% and 70% of women experience this pesky symptom.
Hot flashes are when you have a sudden sensation of being overheated. It can also be accompanied by sweating and flushed skin. Usually hot flashes affect your upper body more (like your neck, face, arms, and chest area).
Why do perimenopausal women get heat flashes?
When estrogen levels drop, it disrupts the function of your hypothalamus. (This is pretty much your body’s internal thermostat.)
Low estrogen causes the hypothalamus to trigger the widening of your blood vessels close to your skin’s surface. This then cues your sweat glands to kick into action and cool you down. (Hence all the sweating!)
3. Disrupted sleep
Sleep disturbances during perimenopause are mostly caused by hot flashes and night sweats. Again, this is triggered by those plummeting estrogen levels.
If you have more severe hot flashes, you are more likely to experience insomnia or challenges with sleep.
4. Vaginal changes
The effects of low estrogen don’t stop with heat flashes and irregular periods (unfortunately). It can also cause you to experience vaginal dryness and irritation. This can lead to discomfort when you go pee or have sex.
This extra dryness can also make you more susceptible to vaginal infections and Urinary Tract Infections (UTIs).
5. Mood changes
As you can imagine, these physical changes are also likely to influence your overall mood. If you’re having hot flashes or sleep interruptions, you may have more mood swings and irritability. And during perimenopause, women are at a higher risk for anxiety and depression.
These mood swings may resemble the way you typically feel before your period (like PMS). But they’re different because they can happen throughout your cycle.
Know more: 4 Phases of Menstrual Cycle and Moods that Go With Each
6. Higher cholesterol levels
You already know that estrogen is vital for the function of your menstrual cycle. But it also has important cardioprotective qualities.
Mainly, it helps with preventing heart disease. This is because it lowers bad cholesterol (LDL) and increases good cholesterol (HDL).
As you can imagine, this doesn’t bode well for perimenopause when estrogen decreases. Many perimenopausal women begin to see an increase in LDL and a decrease in HDL. And overall, this leads to a greater risk of developing heart disease.
7. Nausea
This is one of the lesser understood perimenopausal symptoms. But some women feel nauseous more frequently when they’re in perimenopause.
Potential causes of perimenopausal nausea could be:
- Heat flashes
- Hormonal fluctuations
- Or side effects from medications taken for other symptoms
Know more: Can Perimenopause Cause Nausea?
8. Fatigue
Fatigue is a very common perimenopausal symptom. According to one survey, 66.8% of perimenopausal women reported having fatigue.
Another study puts into perspective women’s experiences of physical and mental exhaustion:
- 46.5% of peri-menopausal women reported this symptom
- 19.7% of the pre-menopausal women reported this symptom
Like premenopausal nausea, the root cause of this symptom isn’t 100% clear. For some, feeling extra sluggish and tired could be a side effect of having sleep disturbances and night sweats. (Makes sense, right?)
Another possibility is that the extra stressors women face when they reach “mid-life” can lead to increased cortisol levels. And having heightened levels of cortisol more frequently can lead to energy depletion.
Know more: The Hidden Struggle: How to Navigate Perimenopause Fatigue
9. Breast tenderness
When your estrogen and progesterone levels fluctuate, it can cause your breasts to feel fuller, swollen, or even painful. (This is similar to breast tenderness you may feel before your period or in early pregnancy.)
10. Weight gain
Weight gain during perimenopause is a potential side effect of a lot of other factors.
Some of these culprits include:
- Reduced muscle mass
- Slower metabolism
- Changing hormones.
- Less physical activity
- Changes in deity
- Sleep disturbances
- Increased stress levels
11. Headaches
Changing levels of progesterone and estrogen can lead to experiencing headaches or migraines.
12. Challenges with conceiving
Since your cycle and ovulation are more irregular, conceiving may be more difficult. This does not mean it’s not possible, but it may take longer, or you may experience extra challenges (like a lower ovarian reserve).
Over 40 and want to have a baby? It’s a good idea to make an appointment with your doctor to discuss your fertility goals.
Know more: Can You Get Pregnant With Perimenopause? Why It’s Possible
Feeling overwhelmed at the thought of all these symptoms? Or already struggling with some of them?
Thankfully, there are ways that you can alleviate many of these symptoms, at least to a degree. More on this in the next section!
How To Manage Perimenopause Symptoms
You’re not alone in experiencing these frustrating pre-menopause symptoms. But we know that doesn’t make it any easier to deal with. After all, some of the symptoms may feel like they’re ruling over your day-to-day life.
The good news is that nowadays, there are many steps you can take to limit the impact these symptoms have on you.
Lifestyle changes
Here are some of the most beneficial lifestyle changes you can make when you’re in or approaching perimenopause:
- Eat a well-rounded diet: Certain foods can help you balance your hormone levels (and boost estrogen)
Learn more: How to Increase Estrogen Naturally: 3 Simple Ways
Get adequate exercise and physical activity: This will help you better maintain a healthy weight and lower cortisol levels
Manage your stress: Try practices like deep breathing, journaling, meditation, yoga, and EFT (tapping)
Get plenty of quality sleep: Going to sleep and waking up on a regular schedule is important. It can even improve your estrogen balance nearly 60%. Your sleep environment is important too. Avoid overstimulation (via things like caffeine and screen time) before trying to sleep.
Quit habits that may have adverse impact on your overall health: Like smoking and consuming alcohol
Symptom-specific ways to cope
Symptom | What you can do |
Irregular periods / unpredictable spotting | Wear a pad or panty liner to keep your underwear from getting stained |
Hot flashes | Look out for things that may trigger or worsen your heat flashes (i.e. alcohol, caffeine, sugary foods, etc.) |
Sleep disruptions | Adopt a consistent schedule and routine for sleep (i.e. stimulation-free bedroom, buffer time between large meals and bedtime, etc.) |
Vaginal changes | Look into using water-based lubes (for sex) and vaginal moisturizers if you feel discomfort from the dryness |
Nausea | Keep meals on the smaller side, steer clear of overly spicy or fatty foods, stay hydrated, drink ginger tea or peppermint tea |
Fatigue | Get plenty of sleep (as best you can) and engage in relaxation techniques (massage, deep breathing, yoga, stretching, etc.) |
Breast tenderness | Make sure your bra is supportive, use ice packs or heating packs as needed |
Weight gain | Eat a hormone-balancing diet, exercise regularly, and reduce stress |
Additional measures to manage symptoms
If you want even more out-of-the-box ways to address your symptoms, you may also:
- Ask your doctor about hormone therapy. There are drug therapies out there—like combination estrogen and progesterone pills and vaginal estrogen—that may help.
- Consider using primrose oil to manage the frequency and intensity of night sweats.
- Consult with your healthcare provider about your health. They can help you find ways to manage conditions like high anxiety, depression, and high cholesterol. Really anything that can support your overall well-being!
Can I Get Pregnant During Perimenopause?
Yes, pregnancy during perimenopause is possible. If you still have ovulatory cycles, then you can conceive.
That said, your chances may not be as high as they were during your 20s and early 30s. One study found that chances of conception from ages 40 – 44 are around 10%. Then from ages 45 – 49, that goes down to closer to 2 – 3%.
But thanks to all sorts of fertility interventions available today, there’s lots of reason to remain hopeful if you’re TTC.
In fact, a CDC report shows that birth rates for women aged 40 – 44 years old have steadily increased since the mid-1980s.
So if you are perimenopausal, no need to feel disheartened at all! Although it is a good idea to check with your healthcare provider for guidance on the best course of action to take for your fertility.
Know more: Can You Get Pregnant With Perimenopause? Why It’s Possible
And this is where the Inito Fertility Tracker can help you. Inito removes the guesswork by tracking all four fertility hormones and confirming actual ovulation. This helps you:
- Spot your fertile window even when cycles fluctuate
- Time intercourse with clarity and confidence
- Detect irregular or missed ovulation
With more unpredictable cycles, every opportunity matters — and Inito helps you make each one count.
FAQs
As you age, your ovarian reserve begins to decline. This will trigger a series of hormonal changes over time. These fluctuations can cause your cycle to become shorter and more irregular.
There’s no one “right” thing to do for yourself during perimenopause. There are lots of pieces to the puzzle when it comes to your overall well-being. So do what you can to take measures that benefit your health and vitality (like eating well, sleeping enough, etc.). And if you begin to have concerns about changes or symptoms, check in with your doctor for more guidance.
The number of tests depends on the irregularity and length of your cycles. For someone with an average cycle length of 30 days, 12-15 tests may be required to track and confirm ovulation.
There are a variety of perimenopausal symptoms that you can experience. Here are some of the most common ones:
- Menstrual cycle changes like irregular periods and anovulation
- Hot flashes and night sweats
- Trouble sleeping and fatigue
- Vaginal dryness
- Weight gain
- Nausea and breast tenderness
The main sign that you are entering pre-menopause (aka perimenopause) is changes to your menstrual cycle. This includes having irregular cycle lengths, periods that are lighter or heavier, and spotting. Tracking your symptoms on the free Inito app can help you keep record of these changes. You can then share that information with your doctor so they can help you determine if you’re premenopausal or not. They can also help you with a treatment plan as you approach menopause.
Was this article helpful?
Perimenopause symptoms, severity, and healthcare seeking in women in the US – NPJ
Perimenopausal Bleeding and Bleeding After Menopause – ACOG
Management of the Perimenopause – PubMed
Perimenopause: From Research to Practice – PubMed
Mood Changes During Perimenopause Are Real. Here’s What to Know – ACOG
The Dynamics of Stress and Fatigue across Menopause: Attractors, Coupling and Resilience – PubMed
Contraception During Perimenopause: Practical Guidance – PubMed