Content table
Have you ever noticed that the date your period starts changes every month? Like, have you ever gotten your period on January 1 and then wondered why the next one didn’t start on February 1?
That would be ideal to keep your period start dates as regular as your paycheck dates. However, that’s not always the way of female hormones. Your period doesn’t necessarily sync up to the calendar date – she’s based instead on your cycle length.
Let’s talk about cycle lengths for a second. The average cycle length is between 21 and 35 days. So, if your period starts on January 1, the next one begins on February 3, and the next on March 8, that is totally normal.
You are still within what’s considered a “regular” menstrual cycle, and there’s no need to be worried.
In fact, 69% of women’s menstrual cycles vary up to 6 days from cycle to cycle, so don’t stress if you’re experiencing slight variations.
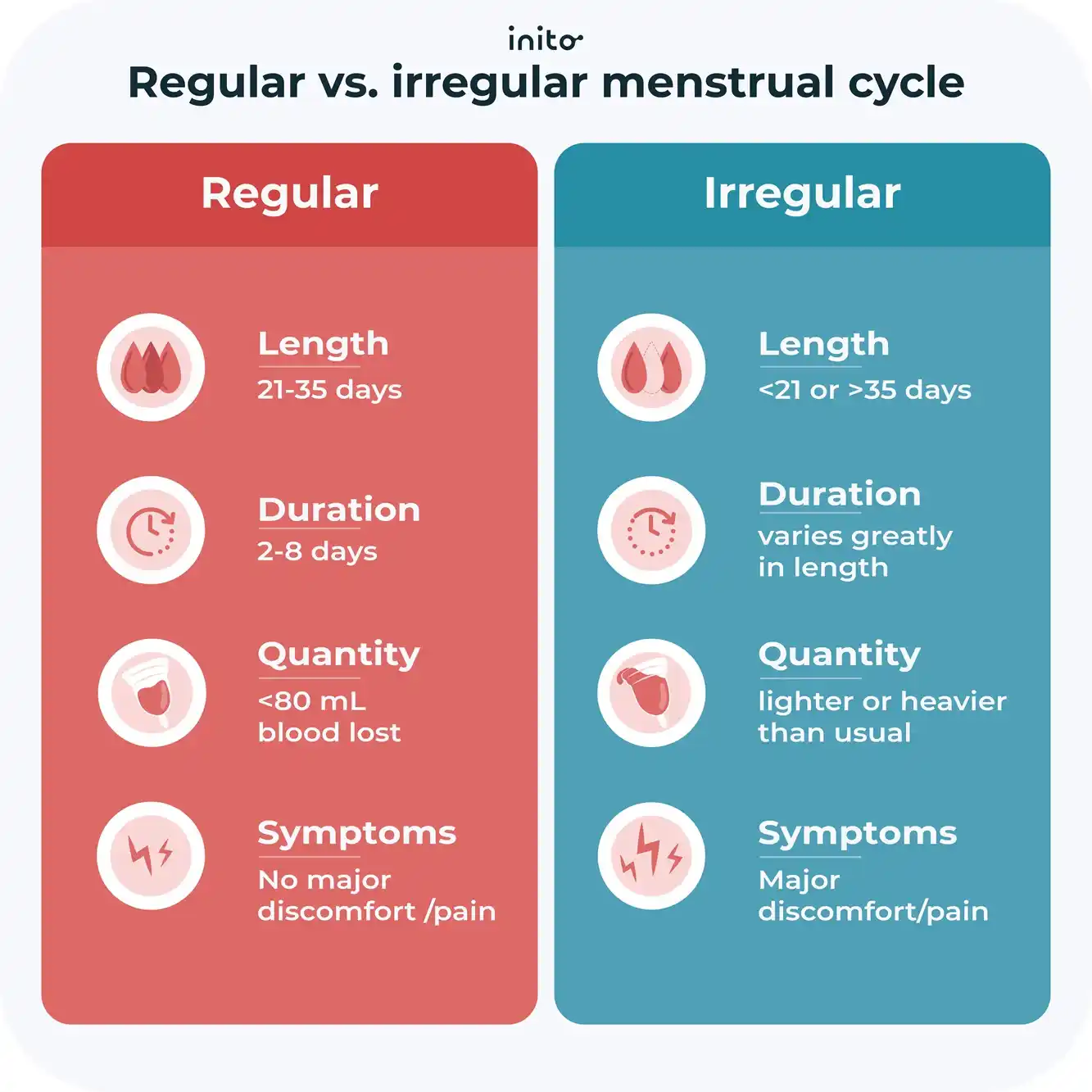
To fall under the category of a “typical” or “regular” menstrual cycle, here’s what you can expect:
- Cycle length of 21-35 days
- Menstruation period of 2-8 days
- An average of 30 mL of menstrual blood lost (but anything less than 80 mL is considered normal)
- No major discomfort or pain
An irregular menstrual cycle is defined by:
- Cycle length of less than 21 days or more than 35 days
- Periods lasting less than 2 days or greater than 8 days
- Cycle length varies significantly from cycle to cycle
- Lighter or heavier flow
- Major discomfort
Okay, now that you’ve got the idea of an average cycle vs. an irregular one, you’re probably feeling a bit better knowing that the slight shifts in your period start dates aren’t something to worry about.
But you may wonder, “Why does my period date change monthly?”
Read on to find out.
Takeaways
- Menstrual cycle start dates can vary monthly and are based on cycle length rather than the calendar.
- A “regular” cycle is 21-35 days long with 2-8 days of menstruation and an average of 30 mL of blood loss.
- The FSH, LH, estrogen, and progesterone hormones control the phases of your menstrual cycle.
- The three main phases of your cycle are the follicular phase, ovulation, and the luteal phase.
- Physiological changes and lifestyle factors, including weight, miscarriage, birth control, stress, excess exercise, PCOS, thyroid disorders, and endometriosis, can cause shifts in your hormones.
- Irregular cycles affect ovulation and conception, but there are things you can do to help.
- You can regulate your cycle by eating a healthy diet, managing your weight, doing the right amount of physical activity, controlling stress, and getting enough sleep.
The #1 reason your period date changes every month
What’s the leading cause of your shifting period date?
HORMONES.
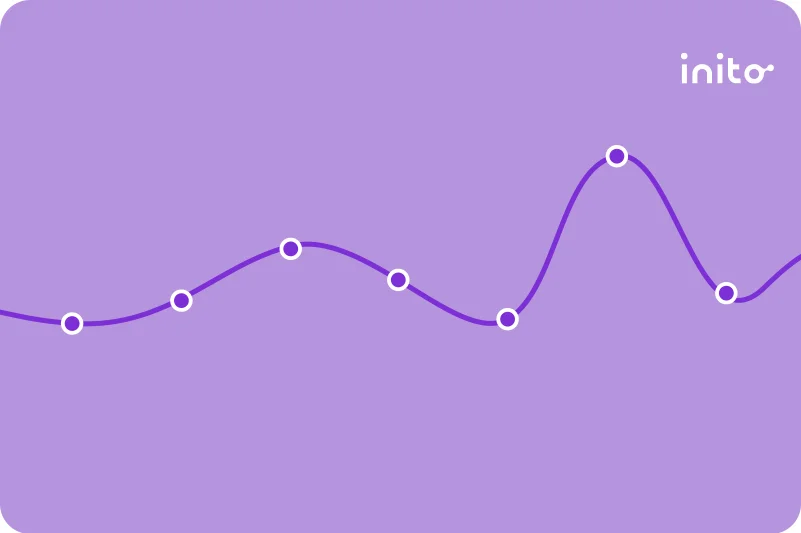
To better understand how these hormones have so much power in deciding when your period starts each month, let’s dive into some of the specifics of the hormone shifts you experience during your cycle, with the help of this chart.
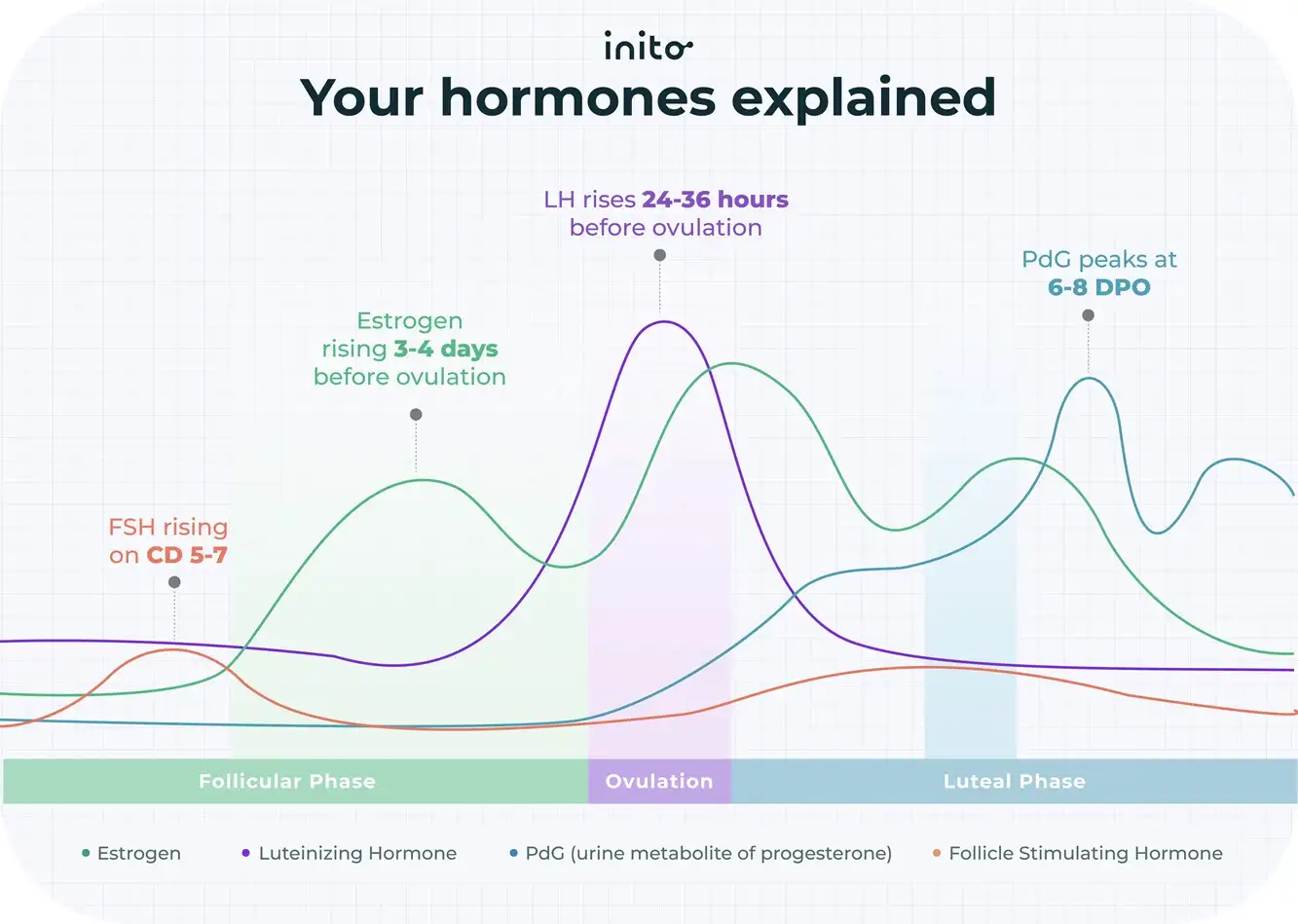
Four hormones are the stars of your period show. They are Follicle-Stimulating Hormone (FSH), Luteinizing Hormone (LH), estrogen, and progesterone. And these hormones fluctuate in each phase of your cycle.
Follicular phase
In the first phase (follicular) of your cycle, your egg matures in the ovaries for possible pregnancy.
Your FSH levels rise, causing the follicles in your ovaries to grow. The lead “dominant” follicle speeds things up, by producing estrogen, causing LH levels to skyrocket and trigger ovulation.
This takes you to the next phase…
Ovulation
Between 24 and 36 hours after your LH surge, your ovary releases a mature egg. And this is when ovulation takes center stage.
This usually occurs 12-14 days before your next period and lasts around a day.
If no sperm shows up, the egg accepts that it’s been ghosted and fades away.
The best way to tell if you are truly ovulating is by using a hormone tracker. The Inito Fertility Monitor tracks all 4 of your key hormones (FSH, estrogen, LH, and PdG) in just one test so you can get a clear picture of where all of your hormones are at.
Luteal phase
After the egg is released, the follicle becomes the corpus luteum, which means it’s time to start pumping out progesterone and estrogen.
These two hormones trigger the inner uterine lining to thicken to prepare for *drum roll please* implantation.
If the sperm is there to fertilize the egg, then the corpus luteum keeps boosting the progesterone. And the placenta then forms right where the fertilized egg implants, which produces progesterone and hCG (Human Chorionic Gonadotropin)).
If the egg isn’t met by sperm, the corpus luteum stops producing progesterone, which leads to the familiar visitor – your period.
As you can see, there are a lot of moving pieces to your cycle, and your hormones are quite sensitive. So, one little shift in your hormones can have a domino effect and change your entire menstrual cycle.
What are some of those shifts you may experience? Let’s find out.
Factors that affect the menstrual cycle
Physiological
Women’s bodies are like a whirlwind of activity, and some of that everyday stuff can get pretty complicated and mess with your cycle, so let’s break it down a bit.
Menarche
Nearly every woman has experienced this, but you may be scratching your head wondering what the heck “menarche” means. It simply refers to your first period ever.
If you remember, your first few cycles were probably irregular and maybe didn’t even happen at all (anovulatory). This means that your period dates were all over the place.
But, chances are good that you were part of the 60-80% of women whose cycles regulated after your third year of menstruating.
Perimenopause
Then, let’s jump to the other end of the period timeline to perimenopause, when your body starts to transition to menopause.
As you get older, your ovarian reserve and estrogen aren’t quite doing what they did in their heyday. So, your body steps in to try and make up for this lack by boosting the production of FSH.
Sounds innocent enough, right? Well, these higher levels of FSH can trigger early ovulation, which means you’re looking at a shorter follicular phase and a shorter time in between periods.
This isn’t necessarily a bad thing if you’re still in the normal range of a 21-35 day cycle. But don’t be surprised if you experience menstrual irregularities during age-related menstrual changes.
Learn More: Signs your Perimenopause is ending and what to do
Breastfeeding

Did you know that breastfeeding can also mess with your menstrual cycle?That’s because when you’re breastfeeding, your prolactin levels are high. This causes your body to suppress the production of FSH and LH.
On top of that, prolactin actually suppresses estrogen and progesterone, which can lead to irregular periods and, oftentimes, even anovulation.
So, if breastfeeding makes your period date all funky, know that with time, your body will restore hormonal balance.
Weight
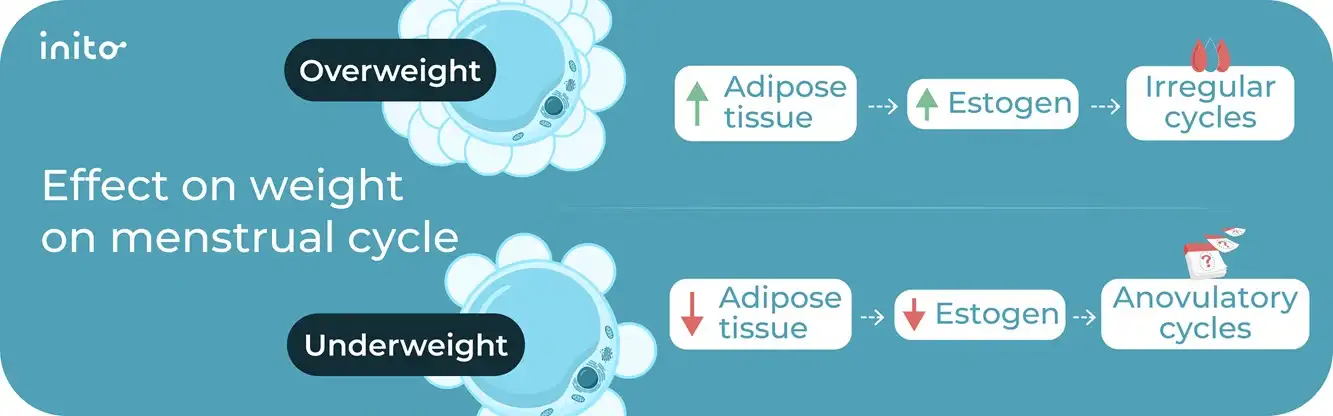
This isn’t the first time you’ve heard that your weight can affect a myriad of things in your body. But it may be the first time you’ve heard that weight can affect your period date.
Overweight and obesity
Studies have found that women who are overweight by 74% of their body weight have 8% of their periods as anovulatory cycles.
But why does this happen?
Because excess weight means more adipose tissue, which boosts estrogen levels too high. This results in lower FSH and LH levels, which causes missed or irregular menstrual bleeding patterns.
Underweight
Being underweight can also affect your period start date.
While modern-day society may give off the idea that skinny = healthy, that’s not always the case when it comes to your period.
Women with a BMI of less than 18.5 have lower fat reserves, which leads to low estrogen production. As a result, the body responds to low estrogen by producing more LH. As LH levels increase, there’s a higher likelihood of anovulatory cycles.
This is seen a lot in women who are competitive athletes and also women who have eating disorders.
(ICYMI – Estrogen is a bit like Goldilocks, where it can’t be too little and can’t be too much but must be just right for regular periods to happen).
So, to keep this from happening, you need to maintain a body fat of at least 22%.
Miscarriage
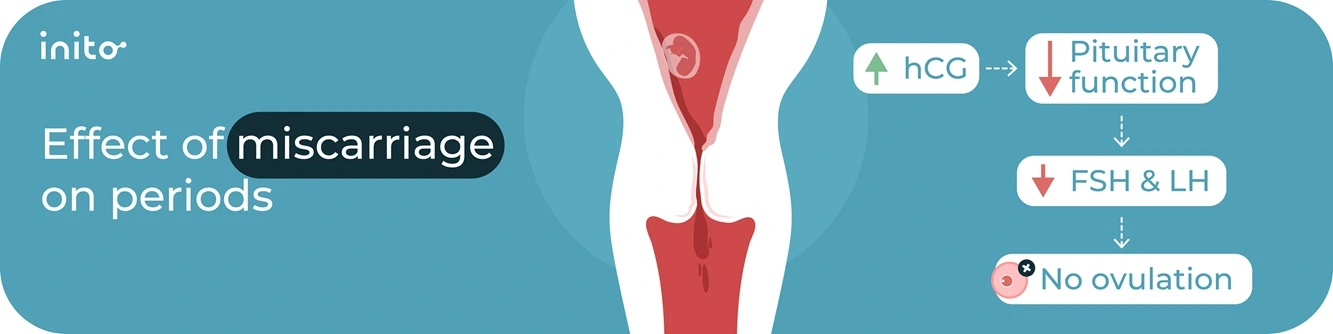
If you’ve experienced a miscarriage, we are so sorry. Words can’t explain how hard and complicated this can be.
Adding to the emotional toll of experiencing a miscarriage, this unfortunate event can also result in shifts in your menstrual cycle timing.
That’s because a miscarriage can make your hCG levels whack. They are pretty high following the loss and can take between 7 and 60 days to return to normal.
How does this affect your period?
High hCG levels prevent ovulation, which means a delayed period.
On top of that, following a miscarriage, your pituitary function drops, which means lower FSH and LH levels, resulting in a shorter LH surge and shorter luteal phase.
You can expect the fluctuation in hormones in this situation to affect your period for 4-8 weeks post-miscarriage. And then you should find hormonal balance.
Stress

Nobody likes stress, but your menstrual cycle really doesn’t like it.
Stress can wreak havoc on your hormone levels, and there are studies to prove it. One study found a direct connection between acute stress and ovulation.
When you experience acute stress, it is far from cute. Your cortisol levels increase along with your LH levels. This means an earlier LH surge and earlier ovulation, which means a shorter cycle.
When that acute stress becomes more prolonged, your cycle shifts differently. The stress hormones block your body from releasing the right amount of LH.
This has the domino effect of reducing estrogen secretion, which means your LH surge gets delayed, and your ovulation gets delayed. This can all end in a delayed cycle and maybe even a missed period.
Increased cortisol levels also cause a reduction in your progesterone levels because the precursor to produce cortisol and progesterone is the same – pregnenolone. This raw material gets used up to produce higher amounts of cortisol. This leads to a decrease in progesterone levels, resulting in shorter cycles.
So, work on that stress reduction to keep your hormones happy.
Excess exercise
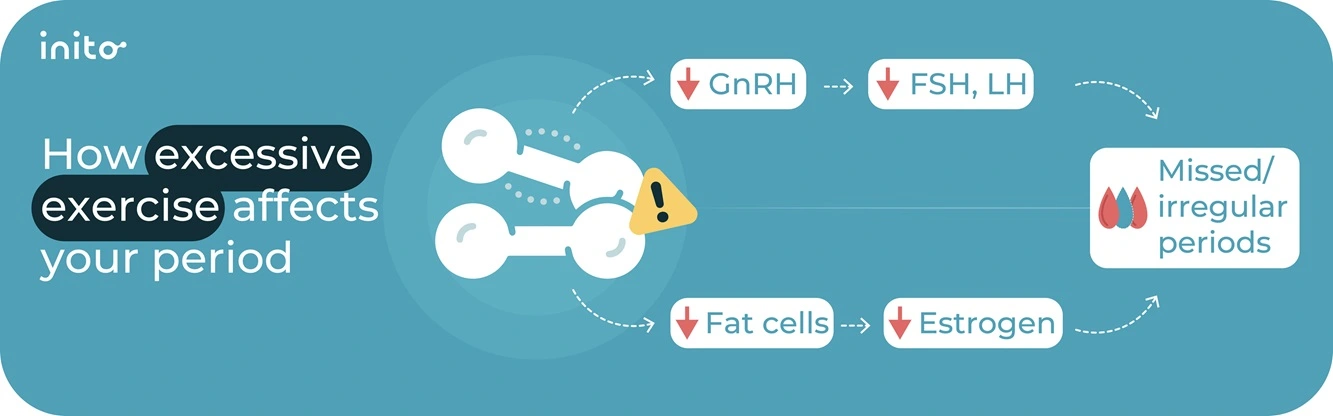
Yes, there is definitely such a thing as working out too much.
You’ve got to find the sweet spot of exercise to keep your hormones happy.
Too much exercise can hinder your hypothalamic function, which can cause your body to secrete less FSH and LH, which means missed or irregular periods.
It can also reduce your fat cells, which can lower estrogen.
So, avoid heavy workouts that last more than an hour to keep your menstrual cycle regular.
PCOS
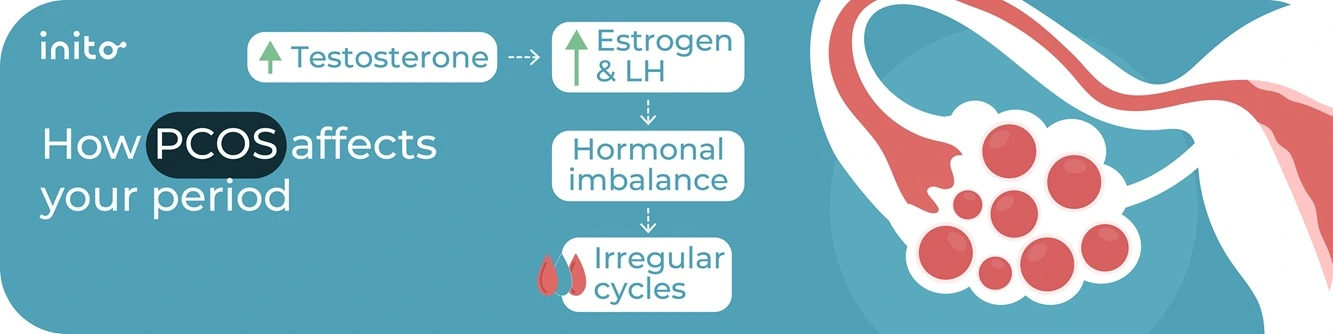
Polycystic Ovary Syndrome (PCOS) is a condition that can make your period date fluctuate.
That’s because PCOS is marked by hyperandrogenism, which is just a fancy way of saying a hormonal imbalance that creates extra male hormones.
These excess male hormones mean abnormally high LH levels in a woman with PCOS, which can lead to insulin resistance as well as keep the ovaries from releasing eggs.
As you can imagine, this means irregular cycles and, in some cases, infertility (though not in all cases – it is possible to get pregnant with PCOS!)
Polycystic ovary syndrome may, in some cases, also lead to struggles with obesity. And, as you have read above, this means more fat reserves, which can skyrocket your estrogen, resulting in an irregular period.
Thyroid disorders

This little butterfly-shaped gland is vital to making and releasing T4 and T3 hormones. And when your thyroid isn’t doing its job correctly, you may find your period start date affected.
That’s because thyroid dysfunction affects the production, transportation, and elimination of both estrogen and progesterone – two key players in your period.
And, your thyroid hormones are stars in the show of follicle growth required for ovulation. With the help of FSH, T3 boosts follicle growth and reduces the death of cells while also reducing the production of too much testosterone and boosting the production of estrogen.
Thus, any issues with your thyroid hormones = issues with ovulation = cycle variations.
Hypothyroidism
This thyroid disorder happens when you’ve got:
- High TSH
- Low T3
- Low T4
- Low SHBG (sex hormone binding globulin)
The affected levels of these hormones can reduce the total circulating estrogen and progesterone in your body, which means – you guessed it – an irregular cycle.
Hyperthyroidism
This branch of thyroid disorders looks like this:
- Low TSH
- High SHBG
And that translates to increased levels of circulating estrogen and progesterone, which messes up your menstrual function, too.
Endometriosis
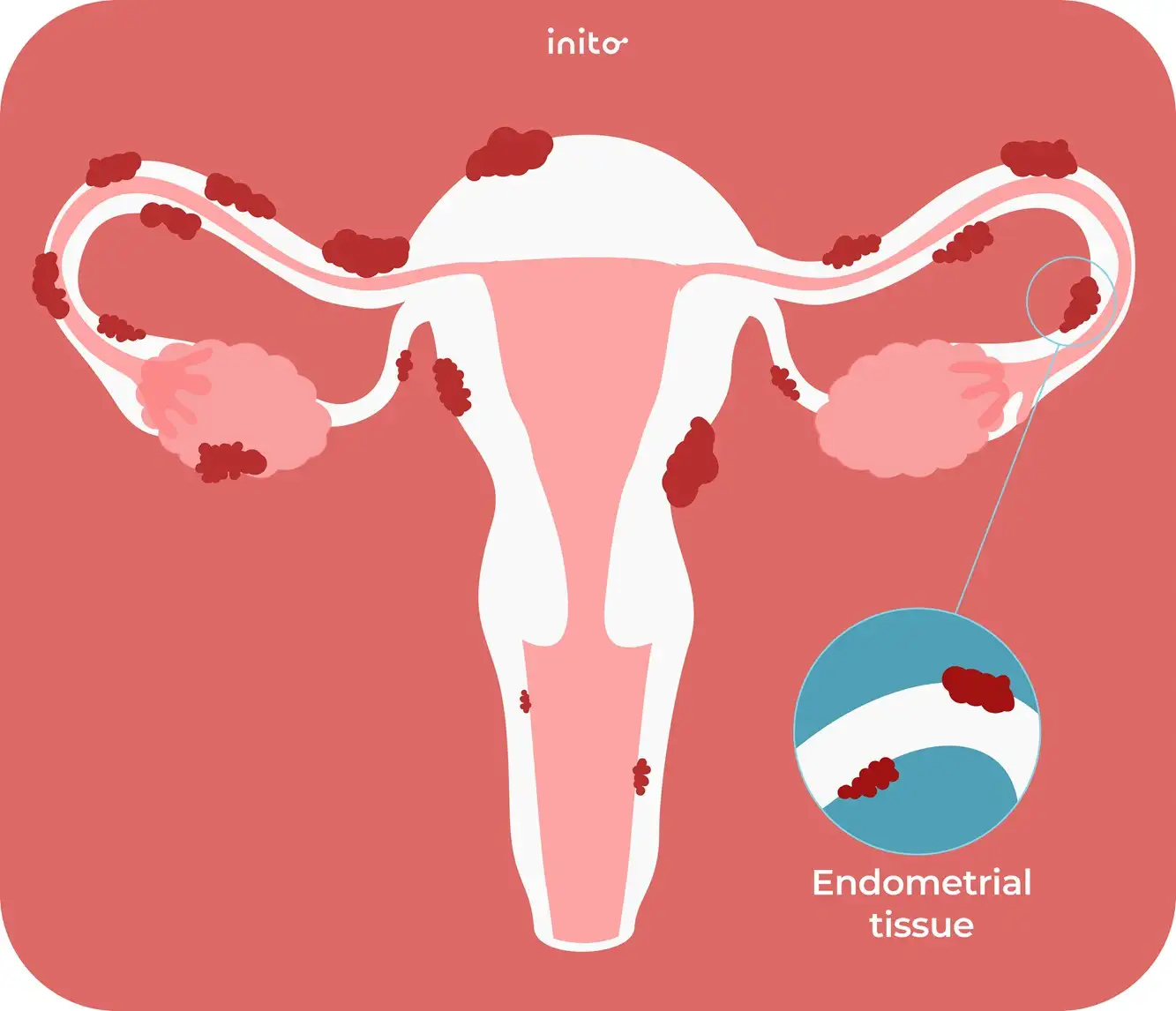
This disorder is the one where tissue that’s similar to what you find in your uterine lining starts to grow outside the uterus, a.k.a, where it doesn’t belong.
As you can imagine, this can cause a range of issues in the body, but in particular, a disruption in the signaling in your body. This leads to:
- Progesterone resistance
- Estrogen dominance
- Irregular ovulation
- Irregular bleeding
- Painful periods
Learn more: Endometriosis vs PCOS: How to Tell The Difference?
Irregular periods and the effect on conception
After all this, you’re likely wondering whether irregular periods can affect your chances of pregnancy.
And the short answer is “yes.” Irregular periods do make it harder to track your ovulation which can make conception more difficult.
However, just because your periods are irregular does not mean you’re not ovulating. Women with irregular periods can still ovulate. The irregularity just makes it harder to know when ovulation happens and, hence, harder to find that coveted fertility window that marks the time for you to get busy in bed.
But don’t lose hope! There are some things that you can do to maximize your chances of conceiving.
Have regular unprotected sex
Though this is kind of aiming in the dark when you don’t know your exact fertile window, the more you do the deed, the more you increase your chances of sometimes getting the timing right.
Tracking your cycles
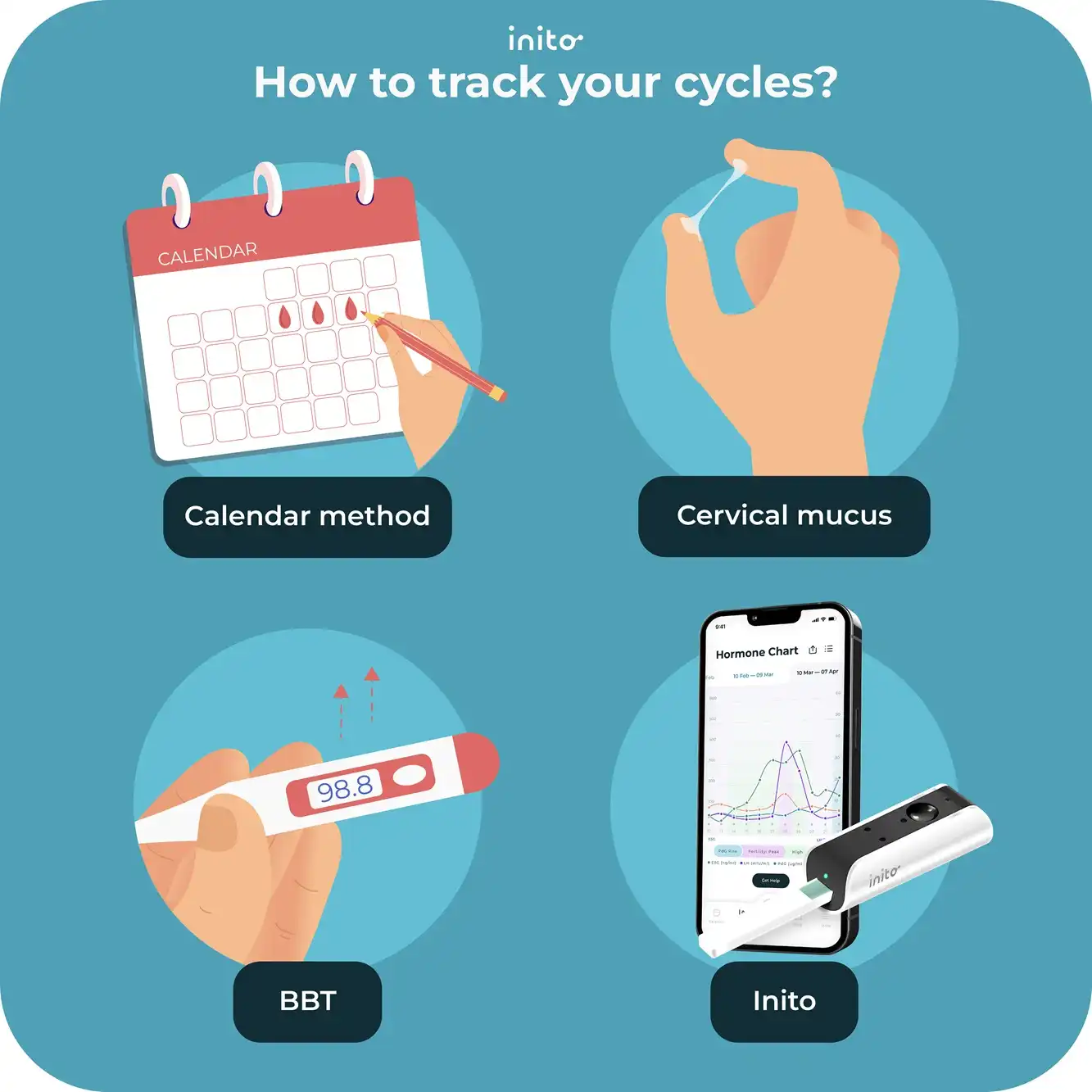
There are four ways to track your menstrual cycle—the good-old calendar method, checking your cervical mucus, tracking Basal Body Temperature (BBT), and Ovulation Predictor Kits or OPKs.
However, the first three methods are unreliable and mostly inaccurate.
- Calendar method: The calendar method doesn’t work for irregular cycles that change from month to month.
- Cervical mucus (CM) method: The CM method is subjective and may not be reliable every month.
- BBT method: BBT can be affected by other things like fever, exercise, and stress. Plus, your BBT only rises the day after ovulation.
- Ovulation Predictor Kits (OPKs): Though OPKs are somewhat reliable, most of them only measure LH, meaning they can predict ovulation but can’t confirm it.
But don’t fear – there’s a solution: The Inito Fertility Monitor.

Inito helps with cycle tracking and can actually confirm your ovulation and fertile window even if you have irregular or skipped periods!
That’s because Inito measures your actual hormone values of FSH, estrogen, and LH, to track your fertile window and PdG (urine metabolite of progesterone) to confirm your ovulation.
Is it possible to get your period on the same date naturally?
The short answer to this? No. You can’t get your period on the same calendar date every month. That’s because your cycle is all about the length and not the calendar date.
Also, the calendar changes every month. Some months are 30 days, some 31, and then you’ve got your girl February who is just 28 (and sometimes 29!).
But, there are things you can do to help regulate your period!

Diet
Eat a well-balanced diet that includes complex carbs, lean meats, and fiber.
You may also want to look into seed cycling to help. And if you have PCOS, avoid xenoestrogens, and boost your diet with fermented foods and omega 3s.
Weight management
It’s important to keep your weight in a healthy place and not let it go too high or too low to maintain that delicate hormonal balance.
If you find yourself in a place of disordered eating, consider reaching out to a professional for assistance; you don’t need to go through this alone.
Physical activity
Aim for 30 minutes of physical activity daily, but don’t do more than 60 minutes of vigorous physical activity, or you risk anovulation.
Stress management
This may look different for everyone, but do whatever you can to minimize stress. Some of our favorites include:
Some of our favorites include:
- Yoga
- Breathwork
- Meditation
- Walking
If your stress feels unmanageable, turn to a mental healthcare professional.
Regular sleep
Sleep is key to healthy hormones and a regular period. In fact, a regular sleep schedule can improve your estrogen balance by 60%! So start going to bed at the same time and waking up at the same time (yes, on weekends, too, when possible).
When to consult a doctor?
When things go wrong, your menstrual cycle isn’t something to take lightly; turn to a doctor for medical advice with the following health conditions:
- Cycle less than 21 days
- Cycle more than 35 days
- Bleeding for less than 2 days
- Bleeding for more than 8 days
- No period for 3+ months
- You’re changing your pad or tampon every hour
- You’re experiencing severe pain, cramps, nausea, and/or vomiting
Was this article helpful?
- The Normal Menstrual Cycle and the Control of Ovulation – Endotext – NCBI Bookshelf
- Physiology, Menarche – StatPearls – NCBI Bookshelf
- The effect of physical activity across the menstrual cycle on reproductive function – PMC
- Factors associated with regularity and length of menstrual cycle: Korea Nurses’ Health Study – PMC
- Real-world menstrual cycle characteristics of more than 600,000 menstrual cycles | npj Digital Medicine
- Life-Style and Reproductive Factors Associated with Follicular Phase Length – PMC
- Obesity and anovulatory infertility: A review – PMC.
- Menstruation in Girls and Adolescents: Using the Menstrual Cycle as a Vital Sign | ACOG Menstrual cycle: What’s normal, what’s not – Mayo Clinic
- Irregular periods – NHS