Content table
It’s estimated that about 11% of couples in the U.S. struggle with trying to get pregnant a second time. Facing secondary infertility can be incredibly challenging. You may feel lost and confused as to why this is happening after one successful pregnancy. But know that you’re not alone.
We are here to shed light on what secondary infertility is, what causes it, and how you can navigate its challenges with support.
Key takeaways
- Secondary infertility is when you are unable to conceive or carry a pregnancy to term after a previous successful pregnancy.
- Both male and female factors can be causes of secondary infertility.
- Female factors include age, ovulation disorders, uterine abnormalities, fallopian tube issues, underlying health issues, and sexually transmitted infections.
- Male factors include sperm production, quality, count, and motility, sexually transmitted infections, and other health issues
- Lifestyle factors like diet, exercise, and stress can impact fertility in both men and women.
- Diagnosing secondary infertility involves an evaluation of both partners. This includes various fertility tests and physical exams.
- Treatment options for second-child infertility vary depending on the underlying cause. But they can include medication, surgery, or in-vitro fertilization.
- Secondary infertility can present great emotional challenges. It’s important to seek support from partners, friends, family, and support groups during this time.
- Consult a healthcare professional if you’ve been TTC with no success for more than a year (under 35) or 6 months (over 35).
What is secondary infertility? How is it different from primary?
Infertility is of two main types: primary and secondary.
Primary infertility is when you’ve been trying to get pregnant for at least a year with no success.
Secondary fertility means a couple who already has a child is having trouble getting pregnant again.
Both forms of infertility present hardships that can be devastating to couples who are trying to conceive (TTC). But understanding the causes may help you improve your chances of pregnancy.
Causes for secondary infertility in women
Primary and secondary infertility share some of the same causes. And it’s important to note that those causes can come from both women and men. Fertility can change with time for both parties involved, too.
Regardless of sex, infertility is not always something you can control. And it is certainly not something to blame yourself or your partner for.
The best thing you and your partner can do is stay informed and avoid pointing any fingers.
Being aware of potential issues is key in navigating your infertility journey. Let’s do a refresh of the steps of conception and the potential issues that can crop up in each step.
Step 1: Egg/follicle formulation
Normally, the conception process starts in the female reproductive system. The beginning of your menstrual cycle is when the pituitary gland secretes follicle-stimulating hormone (FSH). This hormone stimulates the ovaries to develop multiple follicles, each of which contains an egg. One dominant follicle grows the largest.
In the case of associated conditions, things may look different.
- Age: As you age, your ovarian reserve decreases, which can lead to issues with fertility.
- Primary Ovarian Insufficiency (POI): Egg production can also be hindered by POI. This is when a woman’s ovaries stop functioning normally before the age of 40. They produce lower amounts of estrogen and struggle to release eggs regularly. This can lead to infertility.
POI can be caused by factors including:
- Chromosomal abnormalities
- Genetic conditions like Fragile X syndrome
- Treatments like chemotherapy and radiation
- The scarring of ovarian tissue can also cause issues with step 1 of the conception process. This can happen due to endometriosis, polycystic ovary syndrome (PCOS), past surgeries, infections, and multiple cysts.
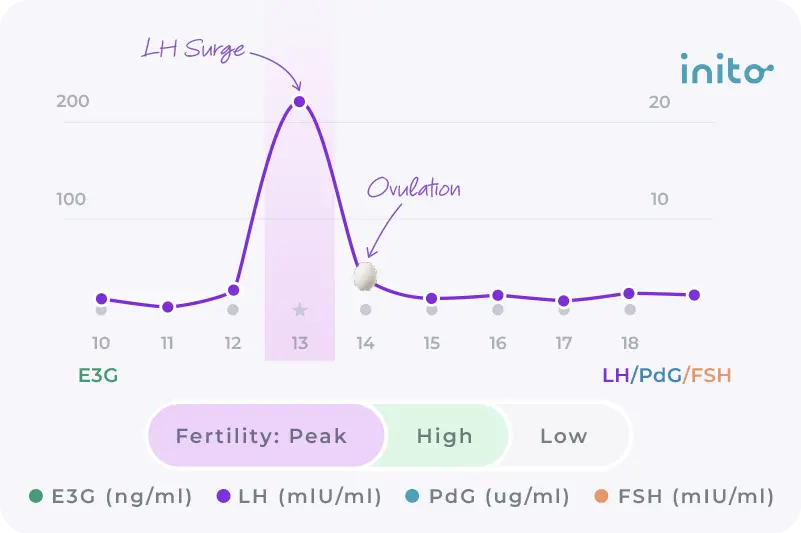
Step 2: Ovulation
The next step of natural conception is ovulation. This is when the dominant follicle releases the egg due to a surge in luteinizing hormone (LH).
However, anovulation can disrupt this step. Anovulation is the absence of ovulation and it can happen due to:
- Polycystic ovary syndrome
- Thyroid disorders
- Hyperprolactinemia
- Being underweight
- Suffering from eating
- disorders
Learn more: Anovulation: Everything you need to know about the #1 cause of infertility
Not sure if you’re ovulating? Inito can help. This fertility monitor tracks your ovulation using four key fertility hormones — LH, estrogen, PdG, and FSH on a single test strip. It predicts your most fertile days and helps confirm whether you’ve ovulated.
Step 3: Fertilization
When things are running smoothly, fertilization happens next. This is when the egg travels down to the fallopian tube to meet the sperm. And fertilization happens.
However, various conditions can keep this from happening. These conditions include:
- Endometriosis
- Infections
- Scar tissue from
- surgeries (i.e. C-section)
- Uterine fibroids
- Polyps
These conditions can lead to blockages in the fallopian tubes or the uterus. This blockage keeps the sperm from reaching the egg. And in this case, fertilization can’t happen.
Step 4: Implantation
The final step in the conception process is when the fertilized egg (now a blastocyst) implants itself in the uterus. This happens around 6-12 days past ovulation (DPO).
But in the case of luteal phase defects, implantation can get tricky. These happen when the body doesn’t produce enough progesterone or can’t respond properly to it. And they can lead to implantation issues. This can increase the risk of miscarriage and an ectopic pregnancy.
Learn more: Your Guide to Luteal Phase Defects
Endometriosis can also present challenges during this step of the process. The inflammation and estrogen dominance associated with endo can interfere with normal implantation.
Now that you’re familiar with the potential challenges of conception, here are other factors that may cause secondary infertility.
- Age
As we talked about earlier, a woman’s fertility and ovarian reserve naturally decline with age. This can make it more challenging to conceive. Additionally, the risk of miscarriages and chromosomal abnormalities rises.
This is a normal part of aging, but we understand it can be difficult. Know that you’re not alone and that there is still hope for a healthy second pregnancy.
- Autoimmune conditions
Sometimes the body’s immune system malfunctions and attacks its own cells. These autoimmune conditions can interfere with fertility and lead to difficulty getting pregnant. These include Hashimoto’s thyroiditis, lupus, antiphospholipid syndrome (APS), etc.
- Unexplained infertility
Some people experience normal test results but still are unable to get pregnant. This is referred to as unexplained infertility.
Now, let’s look at male factors for secondary infertility.
Male causes for secondary infertility
Like we talked about earlier, secondary infertility is not just a female concern. Male factors also play a role in this difficult experience.
Abnormal sperm production, count, morphology (shape), and motility (movement) can all affect sperm quality and thus, a couple’s ability to conceive.
Additionally, low testosterone production, testicular injury, and medical conditions like diabetes, autoimmune diseases, and ejaculatory issues can further affect male infertility.
How do you know what may be causing your secondary infertility? There are a few different ways that doctors can diagnose this infertility in women and men.
How is secondary infertility diagnosed?
Women
Doctors diagnose secondary fertility using fertility tests in different stages of conception.
- Blood tests check hormone levels (FSH and AMH) to evaluate egg production and ovarian reserve, and androgen levels for PCOS.
- Ultrasound scans look at follicular health, uterine health, and ovulation.
- Imaging tests like HSG and hysteroscopy examine fallopian tubes and the uterus for blockages and abnormalities.
- Laparoscopy allows doctors to look at reproductive organs for endometriosis or scar tissue.
Learn more: Your Guide to Navigating Fertility Tests for women
Men
To diagnose male secondary infertility, a semen analysis is done. This looks at sperm count, motility, and overall quality by looking at a semen sample.
Oftentimes the diagnosis also involves a physical exam. This looks for any physical issues and medical history that could point to fertility issues.
How to cope with secondary infertility
The unexpected struggle of secondary infertility can be emotionally difficult. Remember to avoid blaming yourself or your partner.
Rather, focus on maintaining a healthy lifestyle that’s rooted in a balanced diet, exercise, and stress management.
Staying positive and connecting with support groups online and in person can help you navigate this journey. The Inito Facebook group is one such community. Here women share their fertility stories and connect with others experiencing the same struggles.
When to see a doctor
The timeline for seeking advice from a doctor depends on your age.
If you’re under 35 and have been TTC for a year with no success, it’s time to schedule an appointment. The same is the case if you’re over 35 and haven’t conceived after six months.
If you’ve had multiple miscarriages or have a pre-existing condition that could affect fertility, consult your doctor.
FAQs
You may have secondary infertility if you’re TTC and unable to conceive a second child.
The timeline for women under 35 is one year of trying with no success. And the timeline for women over 35 is six months of trying.
Yes, some couples can treat their secondary infertility. The success of a fertility treatment depends on the root of a couple’s fertility struggles.
Treatment options include ovulation-inducing fertility medications (i.e. clomiphene) and in-vitro fertilization (IVF). Doctors may find that surgery in the form of a laparoscopy or testicular surgery may be the right route as well.
There are a few potential reasons you may not be able to get pregnant with a second child.
They include age, blocked fallopian tubes, endometriosis, uterine issues, anovulation, previous pregnancy complications, previous surgery complications, sperm quality, and lifestyle choices.
Research shows that fertility treatments for both primary and secondary infertility often have the same success rates.
However, some factors can make secondary infertility harder to treat. They include age and low sperm count. Note that while these can make treatment more difficult, there is still hope.
You can treat secondary infertility with the help of ovulation-inducing medications, IVF, or surgery.
It’s important to also turn to emotional support during this challenging time. Friends, family, and support groups are key to this experience.
Yes. Secondary infertility is not just a female struggle. Infertility can be caused by males as well.
Was this article helpful?
- Secondary infertility and the aging male, overview | PubMed Central
- Secondary male infertility: the importance of the urological assessment for couples who desire children in later life | PubMed Central
- Primary Ovarian Insufficiency in Adolescents and Young Women | ACOG
- Physiology, Ovulation | NIH
- Implantation Failure in Endometriosis Patients: Etiopathogenesis | PubMed Central
- Managing anovulatory infertility and polycystic ovary syndrome | PubMed Central