Content table
One of the biggest misconceptions about IVF is that the number of eggs retrieved equals the number of babies. But that’s just not true.
In vitro fertilization (IVF) is a complex process with many steps. And at each stage, some “material” gets lost along the way. This is known as the “IVF funnel.”
While this can be disheartening, it’s totally normal. Understanding the process can help you keep realistic expectations if you’re considering IVF.
Keep reading to get the nitty gritty on how the IVF funnel works.
What is the IVF funnel?
In vitro fertilization (IVF) is a fertility treatment where eggs are fertilized by sperm in a lab. The fertilized embryos are then placed inside the woman’s uterus.
However, as mentioned, some material is lost with each step of the IVF cycle.
For example, say a woman starts a cycle with 12 mature eggs retrieved from her follicles. That doesn’t mean she’ll end up with 12 viable embryos for implantation.
Some eggs and embryos don’t make it – for loads of reasons. This is true no matter how you’re conceiving, whether naturally or through assisted reproductive technology (ART). The main difference is that with IVF you get stats along the way.
Attrition is part of the natural selection process. Even so, it can be discouraging. But here’s the upside: Each funnel phase reduces the chances of transferring a non-viable embryo.
Non-viable embryos are more likely to lead to implantation failure or miscarriage. So while the IVF funnel may seem harsh, it serves a purpose.
How is “material” lost at each step of the IVF process?
- Ovarian stimulation. A woman takes injectable hormones that prompt her body to produce multiple eggs.
- Egg retrieval: A fertility doctor removes the eggs from the ovaries during an egg collection procedure.
- Fertilization: The eggs are fertilized in a fertility lab with sperm provided by the partner or donor sperm.
- Embryo growth: The fertility lab monitors the growing embryos for a few days, ideally until they reach the blastocyst stage.
- Embryo transfer: The embryos are then transferred into the woman’s uterus. Approximately two weeks later the woman takes a pregnancy test to check if implantation was successful.
Ovarian stimulation & egg retrieval
As mentioned, hormones are given during ovarian stimulation. This coaxes the ovaries to grow as many follicles as possible. Each follicle is a fluid-filled sac that houses an egg. However, not all follicles develop into mature eggs. Roughly 30% of all eggs retrieved are immature. Immature eggs are more likely to have implantation issues or lead to miscarriage. So they’re not ideal for fertilization. So say a woman goes through ovarian stimulation and ends up with 20 follicles. Out of those 20, about 14 may develop into mature eggs. Why some eggs mature and others don’t isn’t clear. However, age may play a role. Research shows the number of eggs retrieved declines with age, while the number of immature eggs increases. In general, the more eggs retrieved, the higher your chances of an IVF cycle resulting in a life birth. So what’s the magic number? One study compared the pregnancy rates for 1,615 IVF cycles. They found that pregnancy rates were best when at least 10 eggs were retrieved.| Number of eggs retrieved | Pregnancy rate (in %) |
| 1-4 eggs | 30.8% |
| 5-9 eggs | 36.2% |
| 10 or more eggs | 44% or higher |
Fertilization
After the eggs are retrieved, they’re fertilized in a fertility lab. There are two routes here. The first is conventional fertilization. In this case, an egg and sperm are mixed together in a petri dish. The second option is intracytoplasmic sperm injection – or ICSI for short. ICSI involves injecting sperm directly into an egg. No matter which option you choose, typically 70-80% of eggs get fertilized. So if 14 eggs are retrieved, roughly 11 may get fertilized.Embryo development
The fertility lab observes the fertilized eggs over the next few days as they develop into embryos. Embryos typically grow until day 3 or day 5. Day 3 embryos have roughly 8-10 cells, while day 5 embryos (blastocysts) have between 80 to 100 cells. Transferring embryos at the blastocyst stage tends to be more successful than at earlier stages. Even so, not all embryos will grow enough–or be of high enough quality–to be suitable for embryo transfer. Sadly, less than 50% of embryos make it to the blastocyst stage. Many factors play a role here, including laboratory conditions, sperm quality, and egg quality. Meaning, that out of 11 fertilized eggs, only about 6 embryos will survive. Read more: Day 3 vs. Day 5 Embryo Transfer: Which is Better?Genetic testing results
For the embryos that do reach the blastocyst stage, you have the option to do genetic testing. This is called preimplantation genetic testing, or PGT testing. And it tells you whether the embryos are genetically normal. To do PGT testing, you need to freeze the embryos. This adds to the IVF timeline, but since it can offer peace of mind, many find it’s worth the wait. Studies show about 35% of day 3 embryos are genetically normal (euploid), while around 55% of day 5 embryos are genetically normal. This means if 6 embryos reach the blastocyst stage, only about 3 of them may be chromosomally normal. These rates stay the same between ages 24 to 35. However, after age 35, the number of genetically normal embryos drastically decreases. At age 35 roughly 60% of embryos are genetically normal. But by age 40, that number drops to 35%. And by age 45, only about 15% of embryos are euploid. This is where PGT testing can be useful. That way, you know which embryos are the healthiest and have the best chance of implantation. If egg quality is an issue, remember donor eggs are always an option.Embryo implantation
Following embryo transfer comes what many consider the hardest part of IVF: “the two-week wait.” This is the 11-14 days after embryo transfer when you’re waiting to find out if an embryo got attached to your uterine wall. Unfortunately, not all embryos successfully implant. This can make the two-week wait a difficult and nerve-wracking time. Read more: Your Complete Guide to Surviving the Two Week Wait One study found implantation rates per embryo transferred range between 10 to 40%. According to this study, the average implantation rate is about 26%. However, other studies are more encouraging. More on this later. Many factors play a role in whether or not an embryo implants. These include endometrial receptivity, the techniques used during embryo transfer, and embryo quality. Embryos are graded and given a blastocyst morphology score based on the shape and appearance of their cells. Typically, the higher the score, the higher the implantation and live birth rates. To illustrate this, one study looked at embryo quality from 1,766 IVF cycles. Here’s what they found:| Embryo score | Pregnancy rate (implantation rate) | Live birth rate |
| “Good” embryos | 55.6% | 46.8% |
| “Fair” embryos | 47.2% | 39% |
| “Poor” embryos | 43.6% | 34.1% |
| IVF stage | Number of eggs/embryos | Attrition rate | Actual material useful for the next stage |
| Ovarian stimulation | 20 | 30% | 14 |
| Egg retrieval | 14 | 20-30% | 11 |
| Fertilization | 11 | 50% | 6 |
| Embryo growth | 6 | 50% | 3 |
| Embryo transfer | 3 | 60-90% | 1 |
Understanding your chances of IVF success
To start, let’s clear up what “IVF success” means. Simply put, it’s when an IVF cycle results in a live birth.
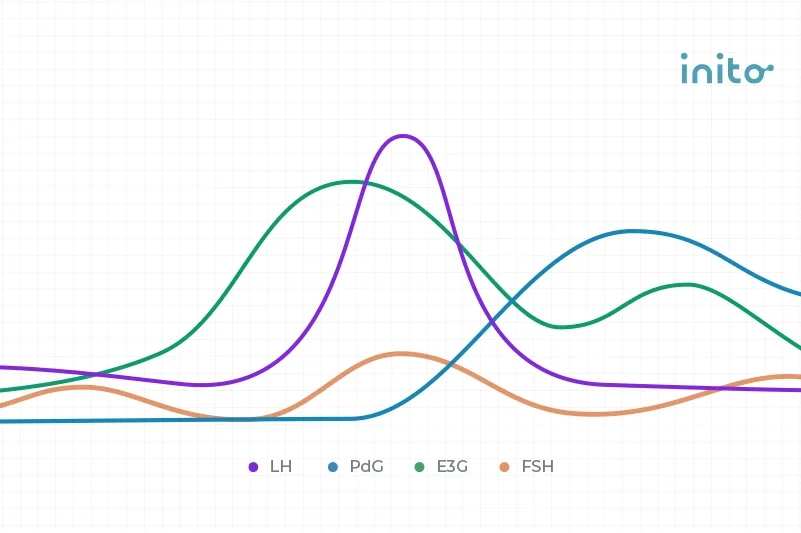
The main factors that affect IVF success rates are age and the quality of the fertility clinic. However, many other things play a role in IVF success. This includes BMI, underlying medical conditions, sperm health, and hormone levels.
This is where understanding your unique fertility characteristics can be a game-changer. This can help you set expectations, reduce stress, and maintain hope throughout the process.
SART (Society for Assisted Reproductive Technology) provides a handy online tool to estimate your chances of IVF success. It compares your data to others with similar profiles and gives predictions based on your:
- Age
- Height and weight
- Number of previous births
- Total number of pregnancies
- Health conditions
- Cause of infertility
While helpful, remember this is just a tool. For a more personalized estimate, talk to your fertility doctor. They can give you an idea of your chances based on your health history, fertility testing, and their experience with patients like you.
Read more: IVF Success Rates: The Factors That Affect Your Chances
The bottom line
Natural selection is part of the IVF process. It’s normal for some eggs and embryos to be lost at each stage.
Each IVF journey is unique. So while it’s hard, try not to compare yours to others. If you start off with a smaller number of eggs or end up with fewer embryos than expected, don’t worry. All it takes is one good embryo to get pregnant.
Research is based on general stats, which vary from person to person. Focus on what’s under your control. Choose a good fertility clinic, eat a healthy diet, and do what you can to reduce stress. That way, your body will have the best chances of IVF success.
Takeaways
- The IVF funnel refers to the natural attrition that occurs during an IVF cycle. At each stage, some eggs and embryos are lost.
- Typically, about 30% of eggs retrieved are immature. Implantation issues and miscarriages are more likely with immature eggs. So they’re not suitable for fertilization.
- Fertilization is successful about 70-80% of the time in IVF.
- Roughly 50% of fertilized eggs develop to the blastocyst stage. At this stage, embryos can be frozen and undergo genetic testing.
- Preimplantation genetic testing (PGT testing) tells which embryos are genetically normal and have the best odds of IVF success.
- Between 35% to 55% of embryos are considered chromosomally normal.
- Implantation is successful for about 10 to 40% of embryos transferred.
- Many factors play a role in IVF success. These include age, the quality of the fertility clinic, health conditions, hormone balance, BMI, and sperm health.
- Navigating fertility challenges and IVF can be overwhelming. But you don’t have to do it alone. If you could use some support on your conception journey, the Inito community is here to help.
Was this article helpful?
- Oocyte Maturity in Relation to Woman’s Age in In Vitro Fertilization Cycles Stimulated by Single Regimen – PMC
- The association between the number of oocytes retrieved and cumulative live birth rate in different female age strata | Scientific Reports
- What is the optimal number of eggs at oocyte retrieval? – Fertility and Sterility
- Total fertilization failure: is it the end of the story? – PMC
- In assisted reproduction by IVF or ICSI, the rate at which embryos develop to the blastocyst stage is influenced by the fertilization method used: a split IVF/ICSI study
- Effects of maternal age on euploidy rates in a large cohort of embryos analyzed with 24-chromosome single-nucleotide polymorphism–based preimplantation genetic screening – Fertility and Sterility
- Implantation rates after in vitro fertilization and transfer of a maximum of two embryos that have undergone three to five days of culture – ScienceDirect
- Factors affecting embryo implantation after human in vitro fertilization: a hypothesis
- Obstetric and perinatal outcomes of singletons after single blastocyst transfer: is there any difference according to blastocyst morphology?
- Impact of Various Parameters as Predictors of The Success Rate of In Vitro Fertilization – PMC