Content table
Getting a positive pregnancy test only to have it turn negative a week later can be confusing, not to mention heartbreaking. But it’s way more common than you think.
If this happened to you, you may have had a chemical pregnancy and we’re sending you lots of hugs. A chemical pregnancy is a very early miscarriage that’s undetectable on ultrasounds. In fact, it happens even before pregnancy symptoms pop up.
So how do you know if you’ve had a chemical pregnancy? And does it affect your fertility?
In this article, we’ll answer those questions and much more. Read on to learn what a chemical pregnancy is, what it looks like, and what to expect after a chemical pregnancy.
Key Takeaways
- Chemical pregnancies are a type of early miscarriage that happens around the 4th or 5th week of pregnancy.
- Chemical pregnancies occur before the gestational sac can be seen on ultrasounds. Instead, they’re diagnosed by declining hCG levels.
- If you take a pregnancy test early and get a positive result but get your period a few days later, you may have had a chemical pregnancy.
- Most chemical pregnancies are due to chromosomal abnormalities. Infections, hormone imbalances, PCOS, diabetes, and thyroid disorders can also increase the risk.
- Since you may ovulate as soon as two weeks after a chemical pregnancy, you can potentially get pregnant again quickly.
- When you’re ready to try to conceive again, you can use Inito to monitor your hormones so you know when you’ll ovulate next.
- There’s no surefire way to prevent a chemical pregnancy. Maintaining hormone balance and addressing untreated health conditions may reduce your risk.
- Chemical pregnancies typically don’t require treatment and resolve naturally.
What Is a Chemical Pregnancy?
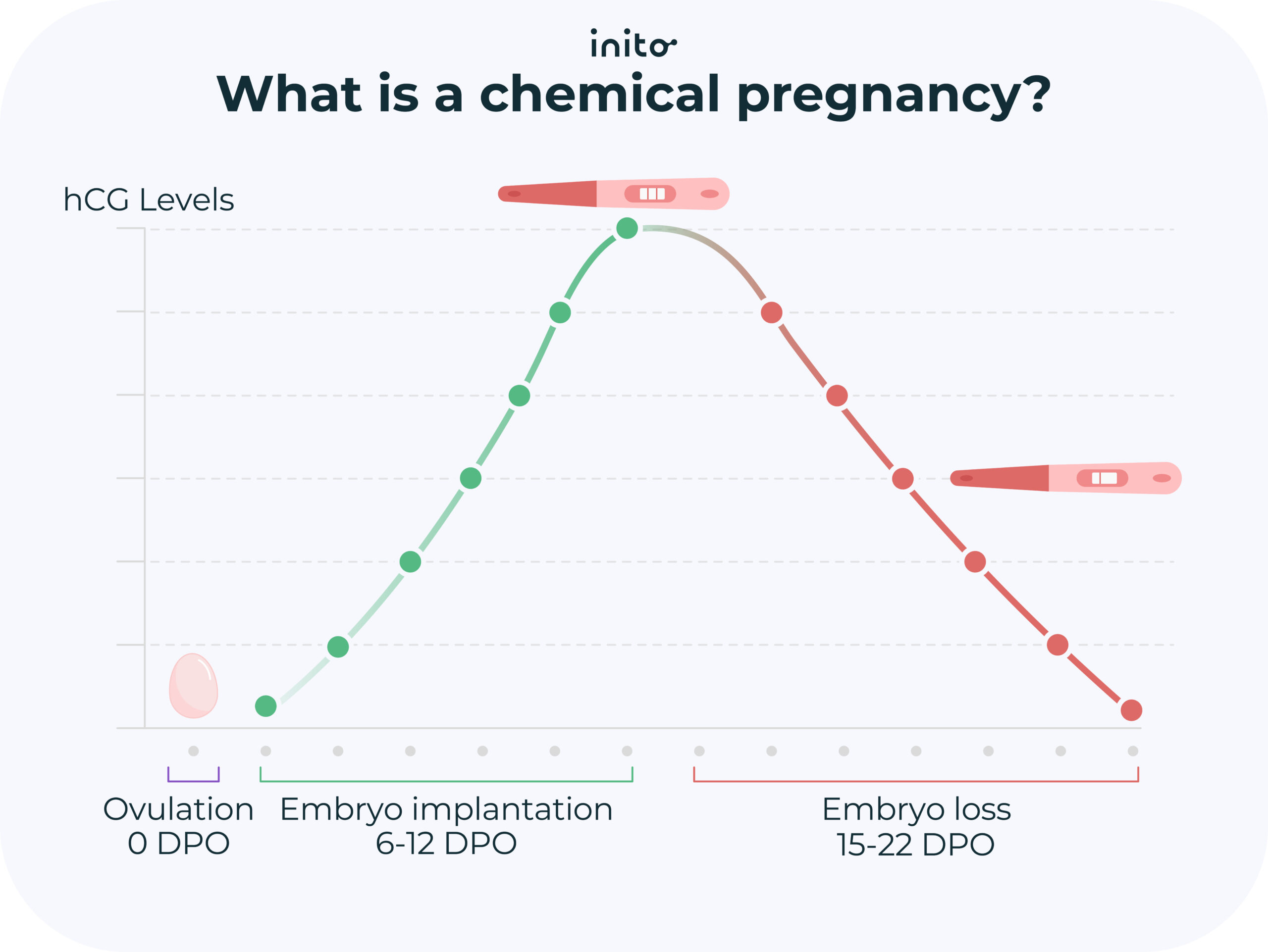
A chemical pregnancy (or biochemical pregnancy) is a miscarriage that occurs early on, before the 5th week of gestation. They happen so early that the gestational sac isn’t even visible on ultrasound scans.
In a regular pregnancy, an embryo forms and implants into your uterine wall. Once implanted, the embryo starts producing human chorionic gonadotropin hormone (hCG). This is the hormone pregnancy tests look for in your urine.
But sadly, in a chemical pregnancy, the embryo stops developing shortly after implantation. This, in turn, causes hCG levels to fall.
Because chemical pregnancies happen before pregnancy symptoms show up, many women are unaware they’ve even had one. You may just assume your period came a bit late.
The name ‘chemical pregnancy’ can sound cold and harsh, and make it feel like it wasn’t a ‘real pregnancy.’ But rest assured, it is. The name simply comes from the hormone hCG that’s used to diagnose it.
How Common Are Chemical Pregnancies?
Very. Some experts say that up to half of all pregnancies end in a chemical pregnancy. And up to 22% of all IVF pregnancies result in chemical pregnancies.
The exact numbers are hard to nail down since many women who have very early miscarriages didn’t even know they were pregnant.
Women undergoing IVF treatments have their hormones tested regularly. So if you’re going through IVF, you’re more likely to recognize if you’ve had one.
If you’re aware you’ve had a chemical pregnancy, it can be devastating. But the silver lining is that it’s proof you can get pregnant.
Most women who go through a chemical pregnancy go on to have a healthy pregnancy the next time. So if you suspect you’ve had one, don’t lose hope!
What Causes a Chemical Pregnancy?

Chromosomal abnormalities are to blame for most early miscarriages, including chemical pregnancies. Typically, an egg and a sperm each contribute 23 chromosomes to the fertilized egg, for a total of 46.
However, sometimes the sperm or egg may contain too many or too few chromosomes. This can make it difficult for the embryo to develop properly or cause problems with implantation. If the uterine lining isn’t thick enough, it can also impair implantation.
Also, sometimes the embryo can get damaged in the IVF freezing process, which can lead to a chemical pregnancy.
In addition, one study suggests chemical pregnancies may be due to problems with angiogenesis, the process which forms new blood vessels.
Since chromosomal abnormalities happen randomly, there’s no way to predict who will have a chemical pregnancy. That said, early miscarriages are more common in women who are 35 or older.
Certain health conditions are risk factors for early pregnancy loss too, including:
- Hormone imbalances
- Having an atypically shaped uterus
- Sexually transmitted infections (STIs) like chlamydia or syphilis
- Polycystic ovarian syndrome (PCOS)
- Diabetes
- Untreated thyroid or blood clotting disorders
Read More: What Does Miscarriage Look Like? Know The Difference Between Miscarriage and Period
What Are the Symptoms of a Chemical Pregnancy?
Since chemical pregnancies happen so early, many women have no symptoms at all.
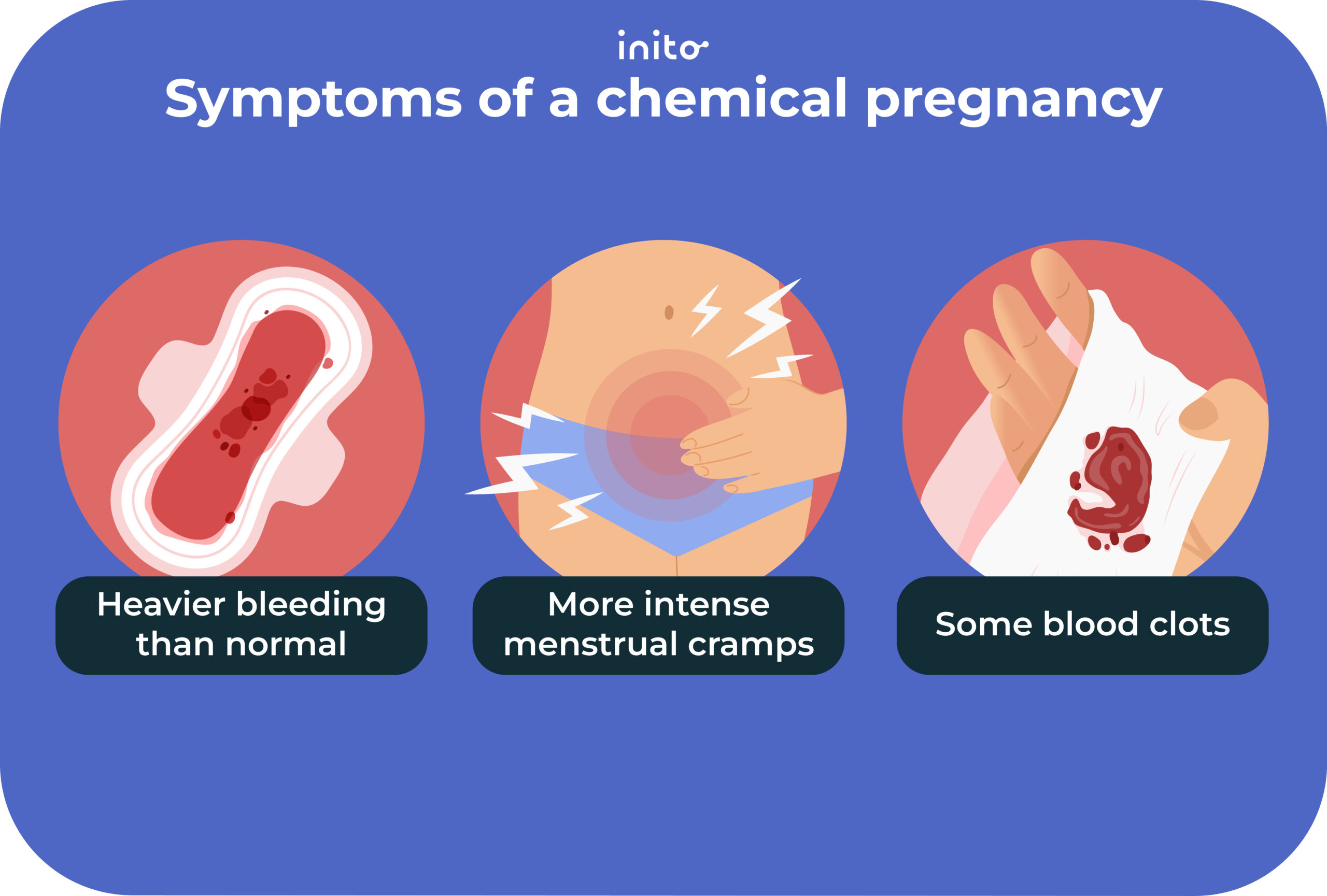
The most common sign of a chemical pregnancy is a late period (roughly a week late). Your period may also look or feel a bit different after a chemical pregnancy. You may have:
- Heavier bleeding than normal
- More intense menstrual cramps
- Some blood clots
But your period alone can’t tell you whether you’ve had a chemical pregnancy. Ultrasounds can’t either since they can’t detect the gestational sac until the 6th or 7th week of pregnancy.
If you suspect you’ve had a chemical pregnancy, taking a pregnancy test is the only way to know for sure.
How Do You Test for a Chemical Pregnancy?

Taking a home pregnancy test can offer clues about whether you’ve had a chemical pregnancy.
Here are a few signs of chemical pregnancy to be aware of, despite testing positive on a pregnancy test:
- You get a negative pregnancy test soon after.
- You get your period.
- You don’t have any pregnancy symptoms like fatigue or nausea.
The only way to confirm a chemical pregnancy is to have your doctor check your hCG levels with a urine or blood test.
If hCG shows up, but your levels are falling, that’s an indication you’ve had a chemical pregnancy.
Read More: Are hCG and Miscarriage Related? A Complete Guide
Getting Pregnant After a Chemical Pregnancy
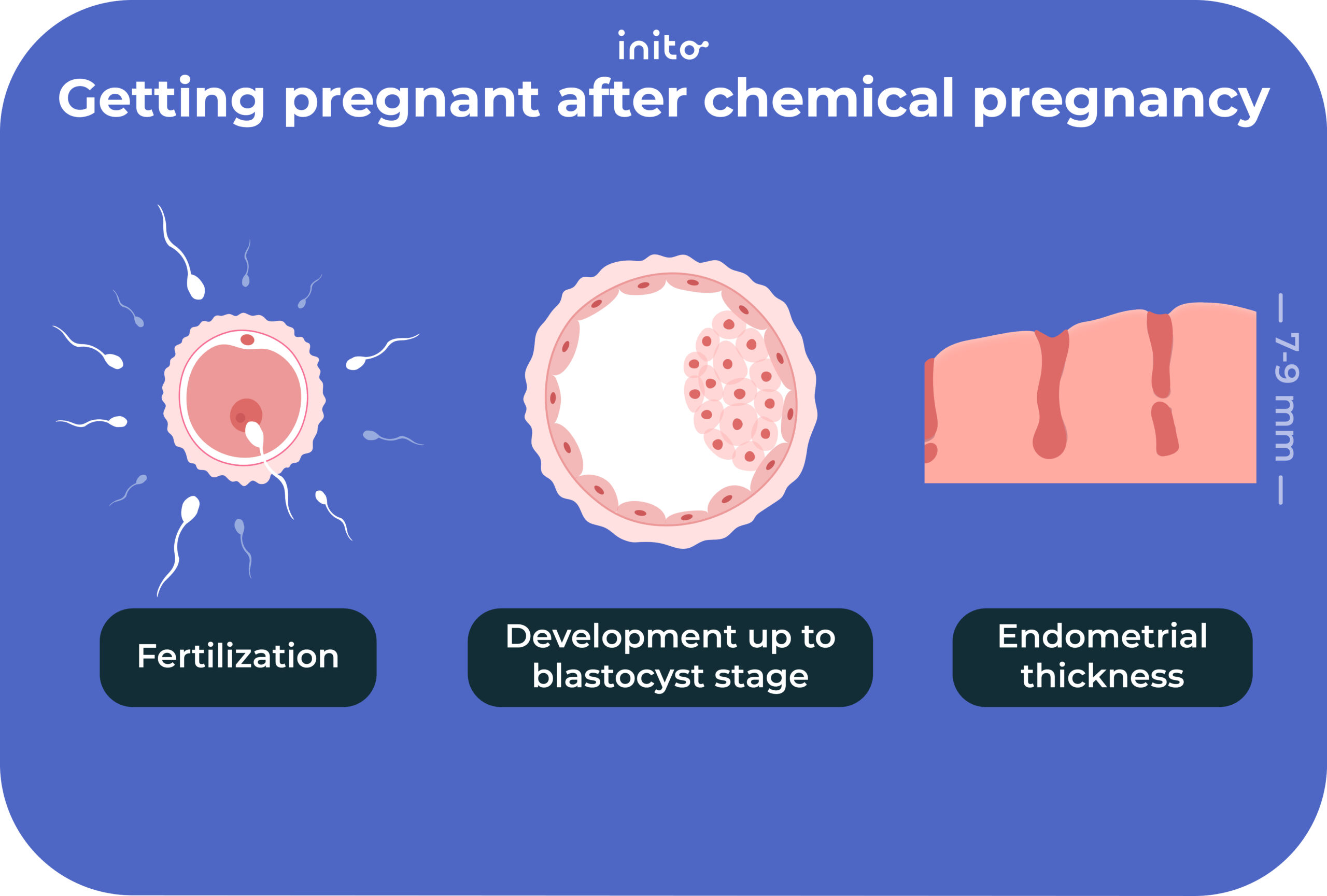
Some women worry that having a chemical pregnancy will make it tough to get pregnant again. But research says just the opposite.
One study compared women who had a chemical pregnancy to those who had a history of negative pregnancy tests. The pregnancy rate in the next cycle for women who had a chemical pregnancy was 38%, compared to 27% for those with repeated negative pregnancy tests.
In another study, couples who tried to conceive within three months after an early miscarriage were 32% more likely to have a successful pregnancy the next time than those who attempted three months later. So know that it can happen.
Ovulation can occur as early as two weeks after an early pregnancy loss. This means you can potentially get pregnant again quite quickly – if you’re ready.
Inito can help you track your fertility hormones, to give you a heads-up when ovulation is on its way. That way, you don’t miss your next chance to conceive.
If you and your partner aren’t ready to try yet and need time to process your loss, honor that. In the meantime, use contraception until you’re ready to try to conceive again.
Read More: Getting Pregnant After Chemical Pregnancy: 6 Helpful Tips
Can You Prevent a Chemical Pregnancy?
Unfortunately, no.
Most chemical pregnancies are due to random chromosomal abnormalities, which can happen to anyone.
That said, you can reduce your risk of chemical pregnancy by addressing any chronic health conditions, such as diabetes, PCOS, or thyroid disorders. That way, you can improve your chances of having a successful pregnancy in the future.
Checking your hormone levels to make sure you are actually ovulating can also help. You can use the Inito Fertility Monitor to keep tabs on your estrogen, FSH, LH, and PdG, a urine metabolite of progesterone, all on a single test strip.
Inito even allows you to download hormone charts you can share with your doctor. This helps you understand any imbalances that may be interfering with your ovulation, so you can make a plan to address them.
Other Types of Miscarriages Besides Chemical Pregnancies
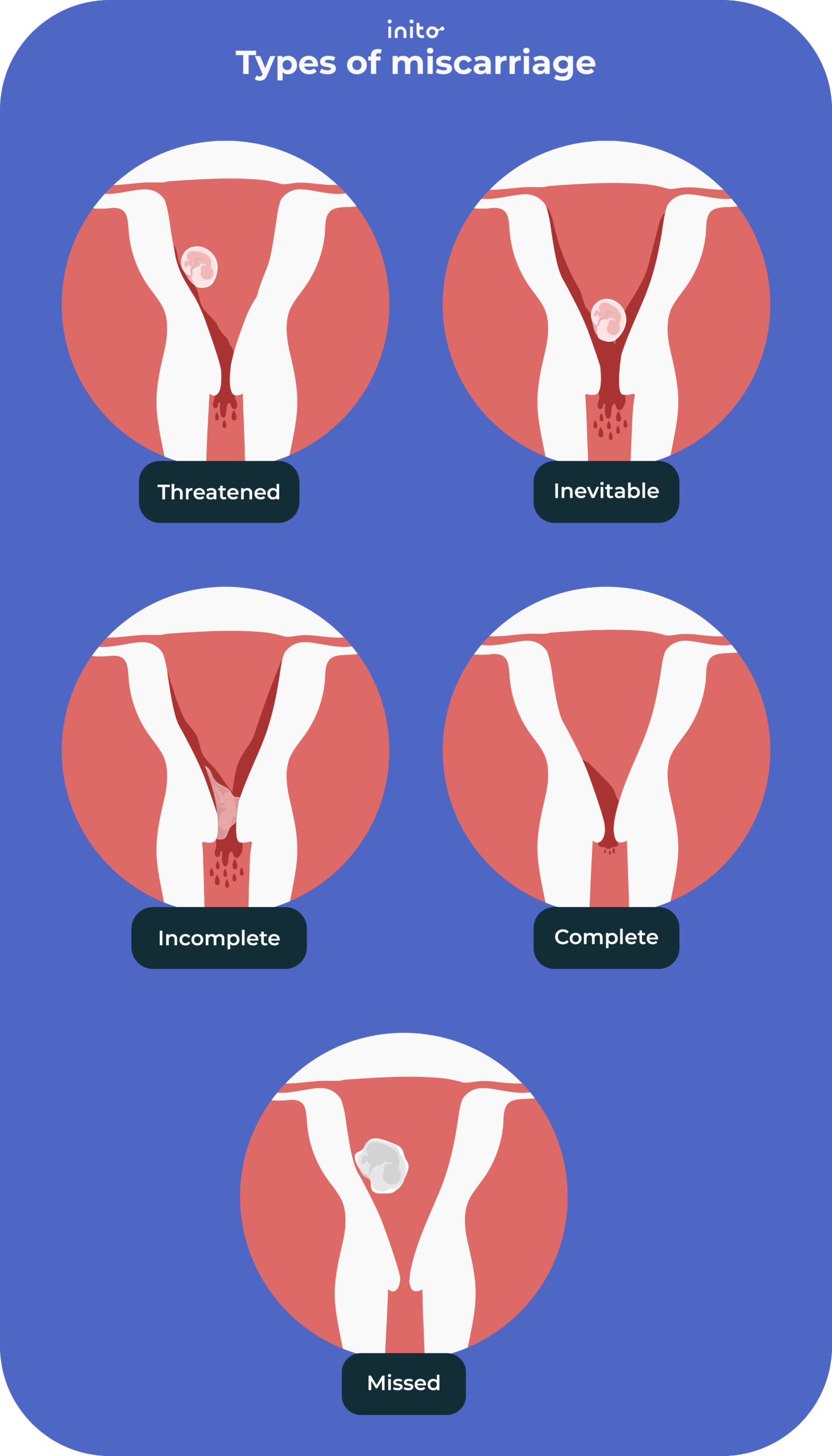
Miscarriages are when a pregnancy ends in the first 20 weeks of gestation. By now, you know a chemical pregnancy is a type of early miscarriage. But there are several other types of miscarriages:
Missed miscarriage
This is when you lose a pregnancy without even realizing it happened. You don’t have any symptoms of miscarriage, like bleeding or pain. But an ultrasound doesn’t detect a fetal heartbeat.
Read More: Silent Loss: Causes and Treatment of Missed Miscarriage
Complete miscarriage
As the name suggests, a complete miscarriage is when your uterus expels all the fetal tissue naturally.
Recurrent miscarriage
This is when you have three or more miscarriages in a row. It’s rare, affecting roughly 1% of women.
Threatened miscarriage
You have vaginal bleeding and/or pelvic cramps during your pregnancy, but your cervix stays closed. 83% of the time, the pregnancy continues. However, you may need to rest more until you recover.
Inevitable miscarriage
You’re having heavy bleeding and cramping, and your cervix starts to open. When this occurs, a complete miscarriage is likely.
When to Visit a Doctor?
Most chemical pregnancies don’t require treatment. Because they occur so early, they tend to resolve naturally, and physical recovery is quick.
Emotional recovery can take longer. Any pregnancy loss can be devastating, no matter how early it happens, especially if you’ve been trying to conceive for some time.
Be patient and allow yourself to feel your feelings. And be sure to get support to process your loss if needed.
If you’ve had more than one chemical pregnancy, talk with your doctor. They can help you address any underlying health conditions that may be affecting your fertility.
Also, if you have a medical condition and suspect it played a role in your early pregnancy loss, consult with your doctor. Getting proper treatment can improve your chances of having a successful pregnancy in the future.
Was this article helpful?
- Biochemical Pregnancy During Assisted Conception: A Little Bit Pregnant – PMC
- Trying to Conceive After an Early Pregnancy Loss: An Assessment on How Long Couples Should Wait
- Early Pregnancy Loss | ACOG
- Etiological evaluation of repeated biochemical pregnancy in infertile couples who have undergone in vitro fertilization – PMC
- Chemical pregnancies: immunologic and ultrasonographic studies